Categories
When should you commit to getting urine?
When can you wait?
When should you forgo testing altogether?
When do I get urine?
Symptoms – either typical dysuria, urgency, frequency in a verbal child, or non-descript abdominal pain or vomiting in a well appearing child.
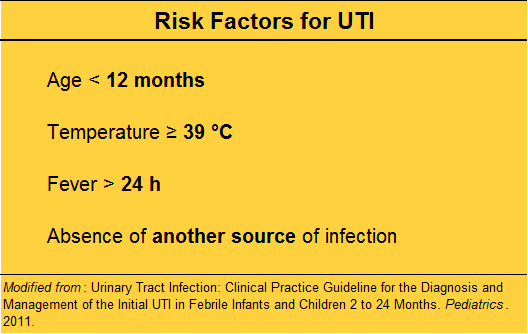
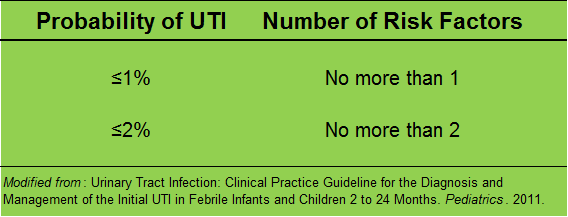
Fever – but first look for an obvious alternative source, especially viral signs or symptoms.
No obvious source?
Risk stratify before “just getting a urine”.
In a low risk child, with obviously very vigilant parents, who is well appearing, you may choose not to test now, and ensure close follow up.
Bag or cath?
The short answer is: always cath, never bag.
(Pros and cons in audio)
What is the definition of a UTI?
According to the current clinical practice guideline by the AAP, the standard definition of a urinary tract infection is the presence of BOTH pyuria AND at least 50 000 colonies per mL of a single uropathogen.
Making the diagnosis in the ED:
The presence of WBCs with a threshold of 5 or greater WBCs per HPF is required.
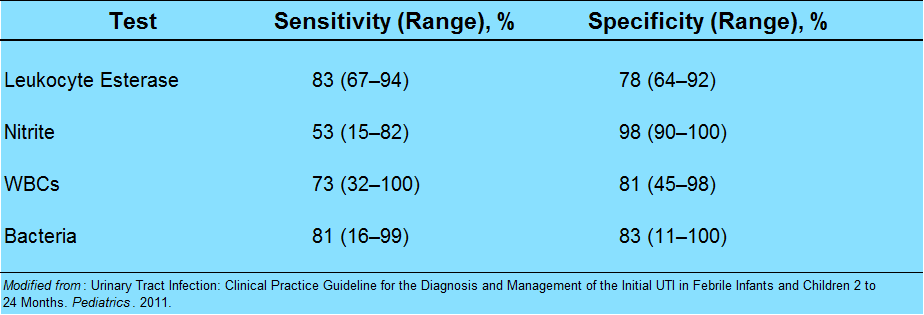
What else goes into the urinalysis that may be helpful?
Pearl: nitrites are poorly sensitive in children. It takes 4 hours for nitrites to form, and most children this age do no hold their urine.
Pearl: the enhanced urinalysis is the addition of a gram stain. A positive gram stain has a LR+ of 87 in infants less than 60 days, according to a study by Dayan et al. in Pediatric Emergency Care.
When can I just call it pyelonephritis?
In an adult, we look for UTI plus evidence of focal upper tract involvement, like CVA tenderness to percussion or systemic signs like nausea, vomiting, or fever. It is usually straightforward.
It’s for this reason that the literature uses the term “febrile UTI” for children. Fever is very sensitive, but not specific in children.
The ill-appearing child has pyelonephritis. The well-appearing child likely has a “febrile UTI”, without upper involvement. However, undetected upper tract involvement may be made in retrospect via imaging, if done.
How should I treat UTIs?
For simple lower tract disease, treat for at least 7 days. There is no evidence to support 7 versus 10 versus 14 days. My advice: use 7-10 days as your range for simple febrile UTI in children.
Pyelonephritis should be treated for a longer duration. Treat pyelonephritis for 10-14 days.
What should we give them?
Sulfamethoxazole and trimethoprim (Bactrim) is falling out of favor, mostly because isolates in many communities are resistant. There is an association of Stevens-Johnson Syndrome (SJS) with Bactrim use. This may be confounded by its prior popularity; any antibiotic can cause SJS, but there are more case reports with Bactrim.
Cephalexin (Keflex): 25 mg/kg dose, either BID or TID. It is easy on the stomach, rarely interacts with other meds, has high efficacy against E. coli, and most importantly, cephalexin has good parenchymal penetration.
Nitrofurantoin is often used in pregnant women, because the drug tends to concentrate locally in the urine. However, blood and tissue concentrations are weak. It may be ineffective if there is some sub-clinical upper tract involvement.
Cefdinir is a 3rd generation cephalosporin available by mouth, given at 14 mg/kg in either one dose daily or divided BID, up to max of 600 mg. This may be an option for an older child who has pyelonephritis, but is well enough to go home.
Whom should we admit?
The first thing to consider is age. Any infant younger than 2 months should be admitted for a febrile UTI. Their immune systems and physiologic reserve are just not sufficient to localize and fight off infections reliably.
The truth is, for serious bacterial illness like pneumonia, UTI, or severe soft tissue infections, be careful with any infant less than 4-6 months of age.
Of course, the unwell child – whatever his age – he should be admitted. Think about poor feeding, irritability, dehydration – in that case, just go with your gut and call it pyelonephritis, and admit.
What is the age cut-off for a urine culture?
In adults, we think of urine culture only for high-risk populations, such as pregnant women, the immunocompromised, those with renal abnormalities, the neurologically impaired, or the critically ill, to name a few.
In children, it’s a little simpler. Do it for everyone.
Who is everyone? Think of the urine rule of 10s:
10% of young febrile children will have a UTI
10% of UAs will show no evidence of pyuria
Routine urine culture in all children with suspected or confirmed UTI up to about age 10
What do I do then with urine culture results?
From a quality improvement and safety perspective, consider making this a regular assignment to a qualified clinician.
Check once in 24-48 hours to find possible growth of a single uropathogen with at least 50 000 CFU/mL. Look at the record to see that the child is one some antibiotic, or the reason why he may not. Call the family if needed.
A second check at 48-72 hours may be needed to verify speciation and sensitivities.
The culture check, although tedious, is important to catch those small children who did not present with pyuria and who may need antibiotics, or to verify that the right agent is given.
Ok, so your UA is negative…now what?
The culture is cooking, but you are not convinced. Below is the differential diagnosis for common causes of pyuria in children: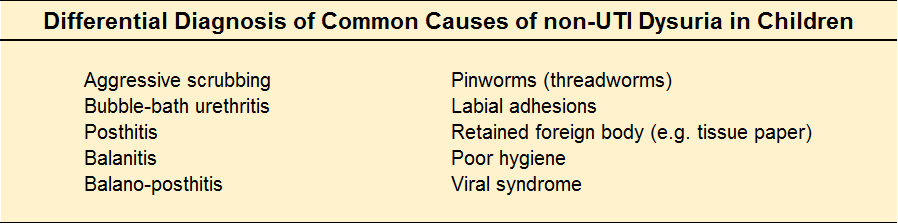
What kind of follow-up should the child get?
The younger the child, the more we worry about missing a decompensation. Encourage the parents to call the child's primary care clinician for a re-check in a few days, and to discuss whether or not further work-up such as imaging is indicated. As always, strict return to ED precautions are helpful.
Who needs imaging?
A more accurate question is: what is an important anomaly to detect?
Vesiculo-ureteral reflux – a loose ureteropelvic junction causes upstream reflux when the bladder constricts.
Uretero-pelvic junction obstruction – in older children or young adults with hematuria, UTI, abdominal mass, or pain. Infants born with UPJ obstruction have congenital hydronephrosis.
Ureterocoele – a cystic mass in the bladder. It is not malignant, but can cause ureteral dilation, and hydronephrosis. Treatment is surgical.
Ectopic ureter – either a duplication of the draining system, or an abnormal connection, such as the epidydimis or cervix.
Posterior urethral valves – occur only in boys, and they are a bit of a misnomer. The most common type of congenital bladder outlet obstruction, posterior urethral valves are just extra folds of membrane in the lumen of the prostatic urethra. Usually ablation by cystoscopy does the trick.
Urachal remnant – a leftover from fetal development, and an abnormal connection between the bladder and the umbilicus. Look for an “always wet” belly button in an infant, or an umbilical mass with pain and fever in an older child.
Imaging of choice as an outpatient?
Renal and bladder ultrasound (RBUS) after the first UTI is recommended (although incompletely followed in practice).
If the RBUS is positive, or with the second UTI, DMSA scan to evaluate possible renal scarring.
So, with all of this testing – are we over doing it?
Like anything, it’s a balance. A few tips to avoid iatrogenia by way of a summary.
If a child over 3 months of age is well, has no comorbidities, has a low grade fever "in the 38s" (38-38.9 °C) without a source, especially if less than 24 hours, you are very safe to do watchful waiting at home.
More to the point, an otherwise well child with an obvious upper respiratory tract infection has a source of his fever.
If your little patient has risk factors for UTI, or you are otherwise concerned, send the UA and send the culture. You can opt out of the culture by middle school in the otherwise healthy child.
And finally, deputize parents to carry the ball from here – the child needs ongoing primary care and his pediatrician may elect to do some screening. Don’t promise or prime them for it – rather, encourage the conversation.
BONUS:
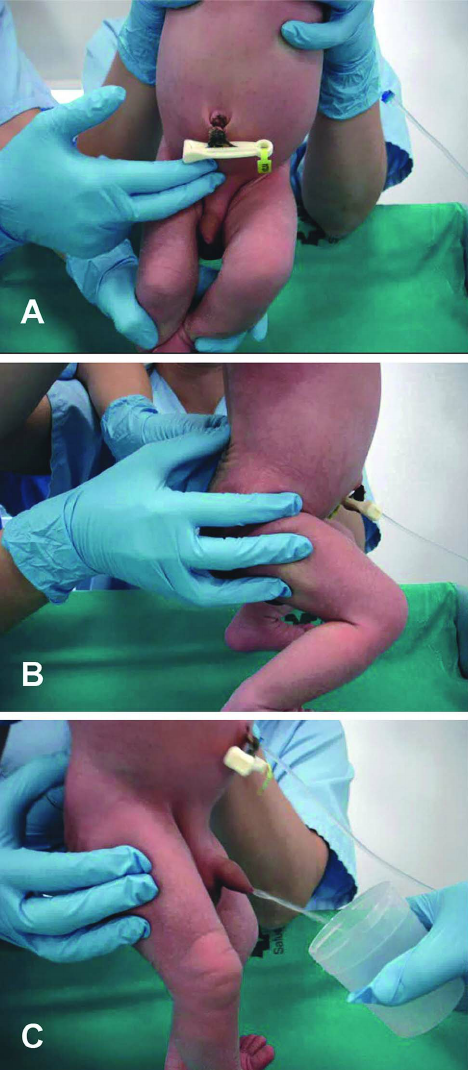
Suprapubic aspiration (details in podcast audio; video below)
BONUS BONUS:
Infant Clean Catch Technique
Step One: feed the baby, wait twenty minutes.
Step Two: clean the genitals with soap and warm water and dry with gauze. Have your sterile urine container open and at the ready.
Step Three: one person holds the baby under his armpits with his legs dangling. The other person gently taps the bladder (100 taps/min), then massages the lower back for 30 seconds.
Step Four: Clean Catch! (can also repeat process)
References
Downs SM. UTI and watchful waiting: the courage to do nothing. Pediatrics. 2014 Mar;133(3):535-6.
This post and podcast are dedicated to Brad Sobolewski, MD, MEd for his innovation and tenacity in all things #FOAMed, #FOAMped, and #MedEd. Thanks, Brad, for your enthusiasm, energy, and for your fantastic PEM Currents and PEM Blog.
Pediatric Urinary Tract Infections
Powered by #FOAMed -- Tim Horeczko, MD, MSCR, FACEP, FAAP