Categories
Does Your Patient Have Streptococcal Pharyngitis?
No Problem -- I'll just Swab.
Not So Fast...
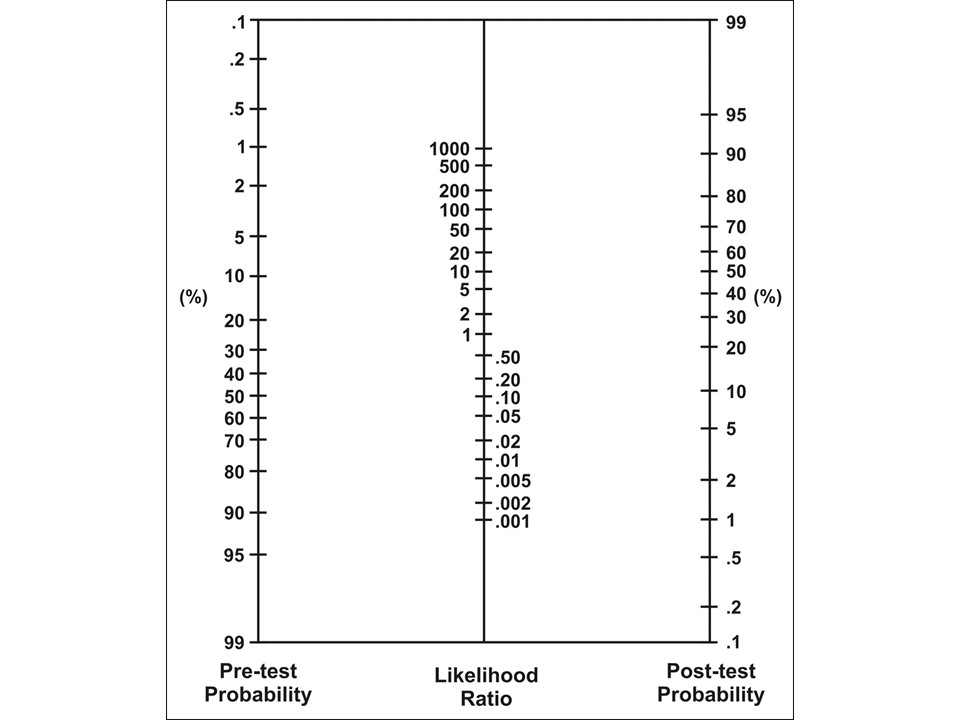
Fagan Nomogram for Likelihood Ratios
1. Decide on your pre-test probability of the disease (choose an approximate probability based on our assessment)
2. Use the likelihood ratio that correlates to your exam.
3. Draw a straight line frm your pre-test probability starting point, to the LR of the feauture/test, take it through to find your post-test probability
4. Use this new post-test probability to help in your decision
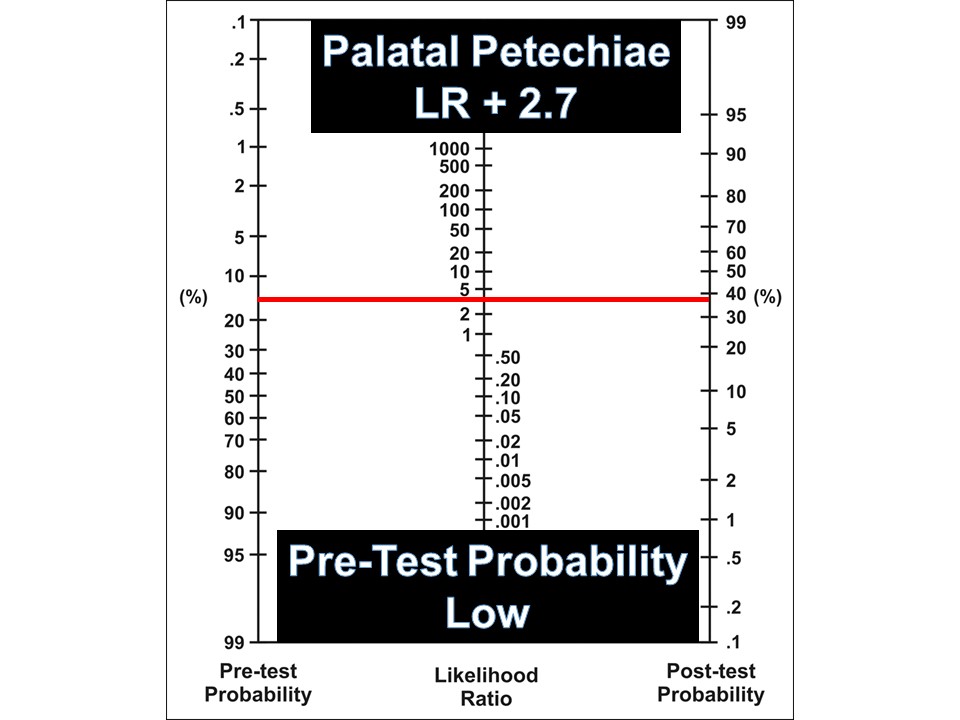
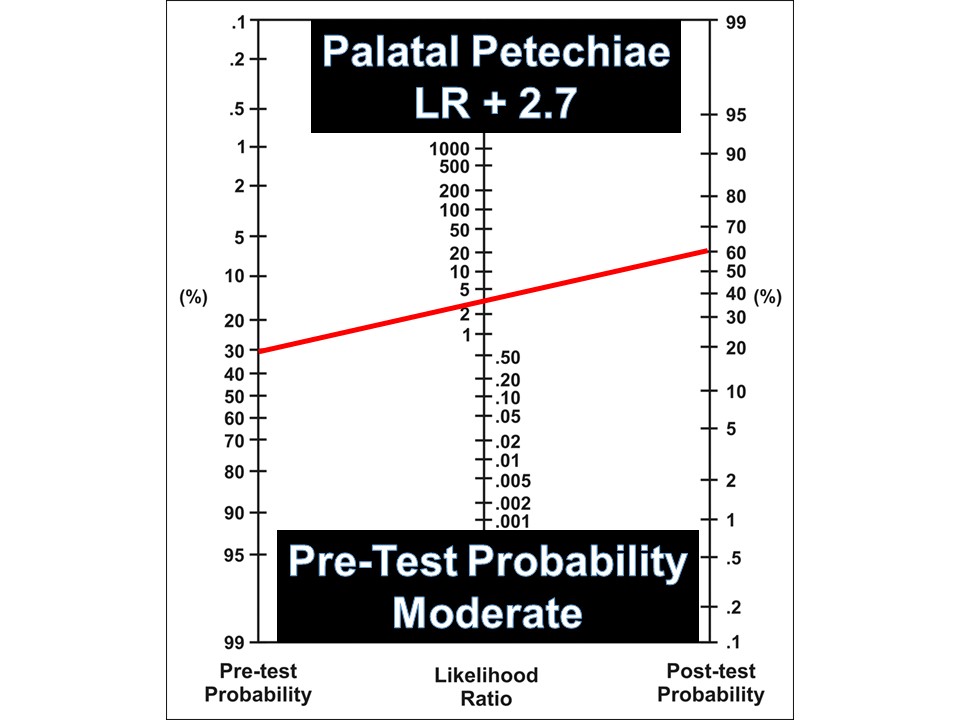
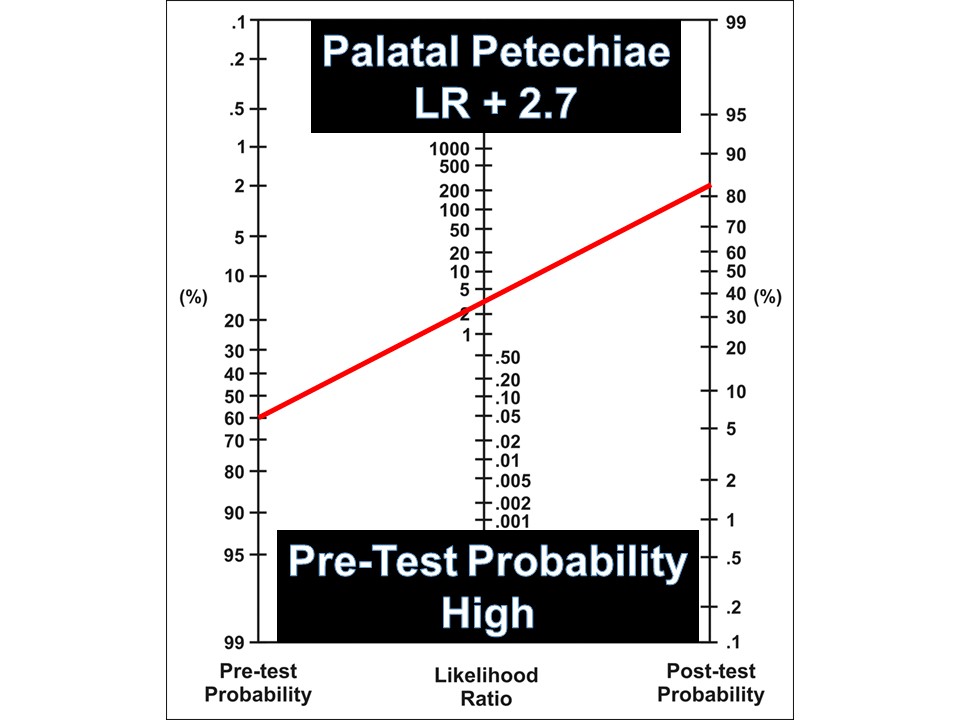
Your patient has palatal petechiae, which confers a positive likelihood ratio (LR+) of 2.7
See below how to use this statistic based on your clinical assessment"
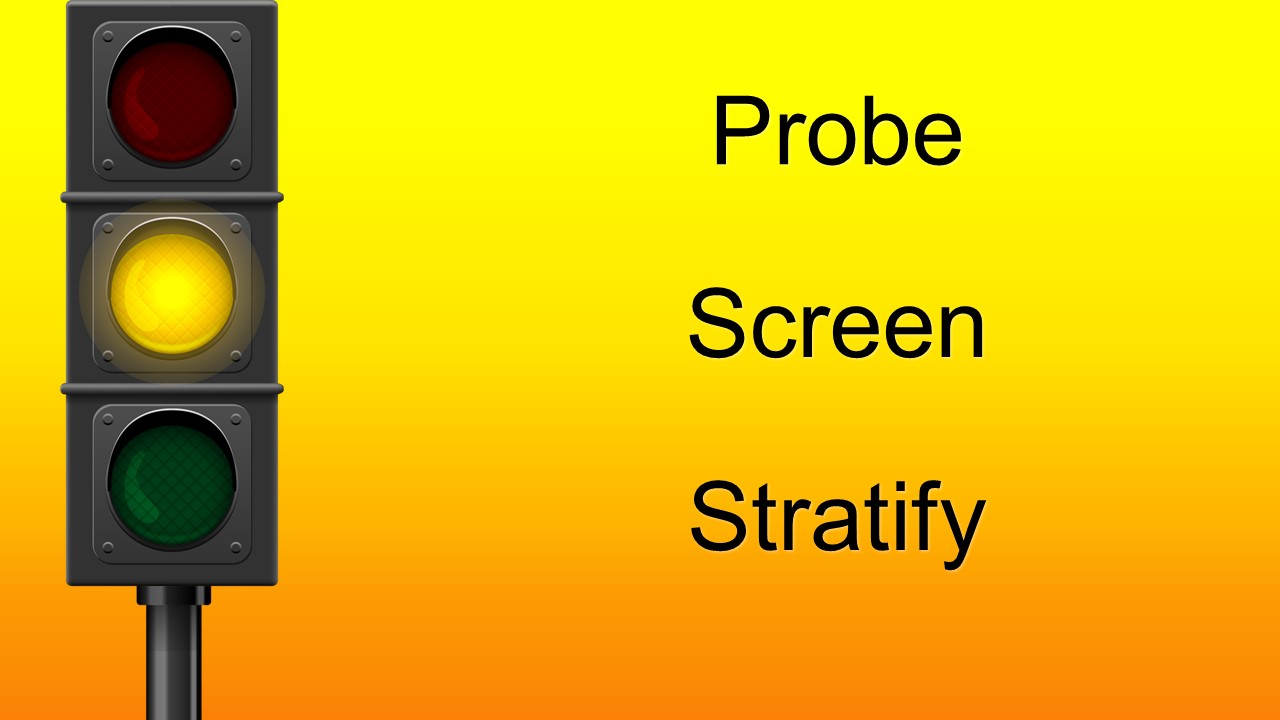
Low Probability
Moderate Probability
High Probability
List of Likelihood Ratios for Streptococcal Pharyngitis
Symptoms and signs | Positive LR (95% CI) | Negative LR (95% CI) | Sensitivity (95% CI) | Specificity (95% CI) |
Scarlatiniform rash | 3.91 (2.00-7.62) | 0.94 (0.90-0.97) | 0.08 (0.05-0.14) | 0.98 (0.95-0.99) |
Palatal petechiae | 2.69 (1.92-3.77) | 0.90 (0.86-0.94) | 0.15 (0.10-0.21) | 0.95 (0.91-0.97) |
Chills | 2.16 (0.94-4.96) | 0.88 (0.79-0.98) | 0.21 (0.18-0.24) | 0.90 (0.83-0.97) |
Anorexia | 1.98 (0.83-4.75) | 0.53 (0.26-1.10) | 0.62 (0.12-1.11) | 0.62 (0.12-1.12) |
Pharyngeal exudate | 1.85 (1.58-2.16) | 0.78 (0.74-0.82) | 0.38 (0.32-0.44) | 0.79 (0.73-0.84) |
Vomiting | 1.79 (1.56-2.06) | 0.85 (0.81-0.90) | 0.28 (0.21-0.36) | 0.84 (0.79-0.89) |
Tender cervical nodes | 1.72 (1.54-1.93) | 0.78 (0.75-0.81) | 0.40 (0.35-0.46) | 0.77 (0.71-0.82) |
Sibling with sore throat | 1.71 (0.82-3.53) | 0.92 (0.82-1.03) | 0.18 (0.14-0.23) | 0.89 (0.83-0.94) |
Halitosis | 1.54 (0.79-2.99) | 0.95 (0.81-1.12) | 0.12 (0.05-0.29) | 0.92 (0.86-0.99) |
Tonsillar and/or pharyngeal exudate | 1.40 (1.10-1.77) | 0.86 (0.75-0.98) | 0.37 (0.28-0.46) | 0.74 (0.68-0.78) |
Large cervical nodes | 1.39 (1.16-1.67) | 0.67 (0.53-0.84) | 0.64 (0.50-0.76) | 0.54 (0.41-0.67) |
Lack of cough | 1.36 (1.18-1.56) | 0.59 (0.48-0.73) | 0.73 (0.66-0.78) | 0.46 (0.38-0.55) |
Tonsillar exudates | 1.35 (0.98-1.87) | 0.81 (0.63-1.06) | 0.46 (0.27-0.67) | 0.66 (0.48-0.80) |
Tonsillar swelling | 1.27 (1.04-1.54) | 0.67 (0.52-0.85) | 0.70 (0.64-0.76) | 0.44 (0.32-0.57) |
Dysphagia | 1.22 (1.00-1.48) | 0.68 (0.51-0.91) | 0.72 (0.55-0.85) | 0.41 (0.23-0.62) |
Headache | 1.22 (0.95-1.57) | 0.90 (0.77-1.04) | 0.39 (0.28-0.51) | 0.68 (0.58-0.76) |
Lack of coryza | 1.21 (1.08-1.35) | 0.69 (0.55-0.88) | 0.72 (0.64-0.79) | 0.40 (0.34-0.48) |
Abdominal pain | 1.18 (0.92-1.51) | 0.95 (0.89-1.03) | 0.24 (0.19-0.30) | 0.79 (0.75-0.83) |
Red tonsils and/or pharynx | 1.13 (0.96-1.33) | 0.41 (0.16-1.02) | 0.93 (0.85-0.96) | 0.18 (0.09-0.35) |
Reported fever | 1.07 (0.96-1.19) | 0.86 (0.67-1.11) | 0.71 (0.58-0.82) | 0.33 (0.23-0.49) |
Red tonsils | 1.07 (0.86-1.34) | 0.82 (0.40-1.69) | 0.80 (0.60-1.00) | 0.25 (0.00-0.51) |
Red pharynx | 1.06 (0.95-1.18) | 0.56 (0.27-1.17) | 0.93 (0.81-0.98) | 0.12 (0.03-0.34) |
Documented temperature >38° or >38.5°C | 1.02 (0.87-1.21) | 0.98 (0.83-1.15) | 0.50 (0.36-0.63) | 0.51 (0.38-0.65) |
Summer | 0.86 (0.61-1.20) | 1.02 (1.00-1.05) | 0.13 (0.00-0.33) | 0.85 (0.65-1.04) |
Arthralgia | 0.74 (0.18-3.08) | 1.02 (0.97-1.06) | 0.09 (0.00-0.25) | 0.90 (0.77-1.04) |
Conjunctivitis | 0.73 (0.46-1.16) | 1.02 (0.98-1.05) | 0.05 (0.02-0.11) | 0.94 (0.85-0.98) |
Acute otitis media | 0.65 (0.14-2.91) | 1.04 (0.93-1.16) | 0.03 (0.01-0.05) | 0.94 (0.84-1.04) |
History of tonsillectomy | 0.64 (0.49-0.84) | 1.07 (1.03-1.11) | 0.11 (0.08-0.13) | 0.84 (0.81-0.86) |
Hoarseness | 0.62 (0.46-0.83) | 1.04 (1.03-1.06) | 0.06 (0.03-0.12) | 0.90 (0.85-0.93) |
Diarrhea | 0.51 (0.33-0.79) | 1.04 (0.99-1.11) | 0.03 (0.00-0.06) | 0.93 (0.86 |
Modified from: Shaikh et al. 2012
This post and podcast are dedicated to Sarah Werner for her constant encouragement of the story in all of us. Check out Write Now with Sarah Werner.
Selected References
Cheung L et al. Throat swab have no influence on the management of patients with sore throats. J Laryngol. 217; 131:977-981.
Ebell MH et al. Rational Clinical Examination: Does This Patient Have Streptococcal Pharyngitis? JAMA. 2000;284(22):2912-2918
Homme JH et al. Duration of Group A Streptococcus PCR positivity following antibiotic treatment of pharyngitis. Diagn Microbiol Infect Dis. 2018 Feb;90(2):105-108.
Nakhoul GN et al. Management of Adults with Acute Streptococcal Pharyngitis: Minimal Value for Backup Strep Testing and Overuse of Antibiotics. J Gen Intern Med. 2013 Jun; 28(6): 830–834.
Oliver J et al. Group A Streptococcus pharyngitis and pharyngeal carriage: A meta-analysis. PLoS Negl Trop Dis. 2018 Mar 19;12(3):e0006335.
Shaikh N, Leonard E, Martin JM. Prevalence of streptococcal pharyngitis and streptococcal carriage in children: a meta-analysis. Pediatrics. 2010 Sep;126(3):e557-64.
Shaikh et al. Accuracy and Precision of the Signs and Symptoms of Streptococcal Pharyngitis in Children: A Systematic Review. J Pediatrics. 2012; 3:487-493.e3
How do we make the diagnosis?
What now?
Concussion in Sport Group Guidelines
Concussion Recognition Tool (for coaches, trainers on field)
Child Sports Concussion Assessment Tool, 5th Ed. (Child SCAT); Ages 5-12
Sports Concussion Assessment Tool, 5th Ed. (SCAT5); Ages 13 and Up
This post and podcast are dedicated to the great K Kay Moody, DO, MPH for her stalwart effort to care for both patient and doctor. Thank you for all that you do to help us to be our best and for promoting #FOAMed #FOAMped and #MedEd.
References
Churchill NW et al. The first week after concussion: Blood flow, brain function and white matter microstructure. Neuroimage Clin. 2017; 14: 480–489.
Ellis MJ et al. Psychiatric outcomes after pediatric sports-related concussion. J Neurosurg Pediatr. 2015; 16:709-718.
Graham R et al. and the Committee on Sports-Related Concussions in Youth; Board on Children, Youth, and Families; Institute of Medicine; National Research Council. Sports-Related Concussions in Youth: Improving the Science, Changing the Culture. Washington (DC): National Academies Press (US); 2014 Feb 4.
Harmon KG et al. American Medical Society for Sports Medicine position statement: concussion in sport. Br J Sports Med. 2013; 47:15-26.
McCrory P et al. Consensus statement on concussion in sport—the 5th international conference on concussion in sport held in Berlin, October 2016. Br J Sports Med. 2016
Purcell LK et al. What factors must be considered in “return to school” following concussion and what strategies or accommodations should be followed? Br J Sports Med. 2018; 0:1-15.
Wang KK et al. An update on diagnostic and prognostic biomarkers for traumatic brain injury. Exp Rev Molec Gen. 2018; 18(2):165-180.
Wang Y et al. Cerebral Blood Flow Alterations in Acute Sport-Related Concussion. J Neurotrauma. 2016 Jul 1; 33(13): 1227–1236.
References
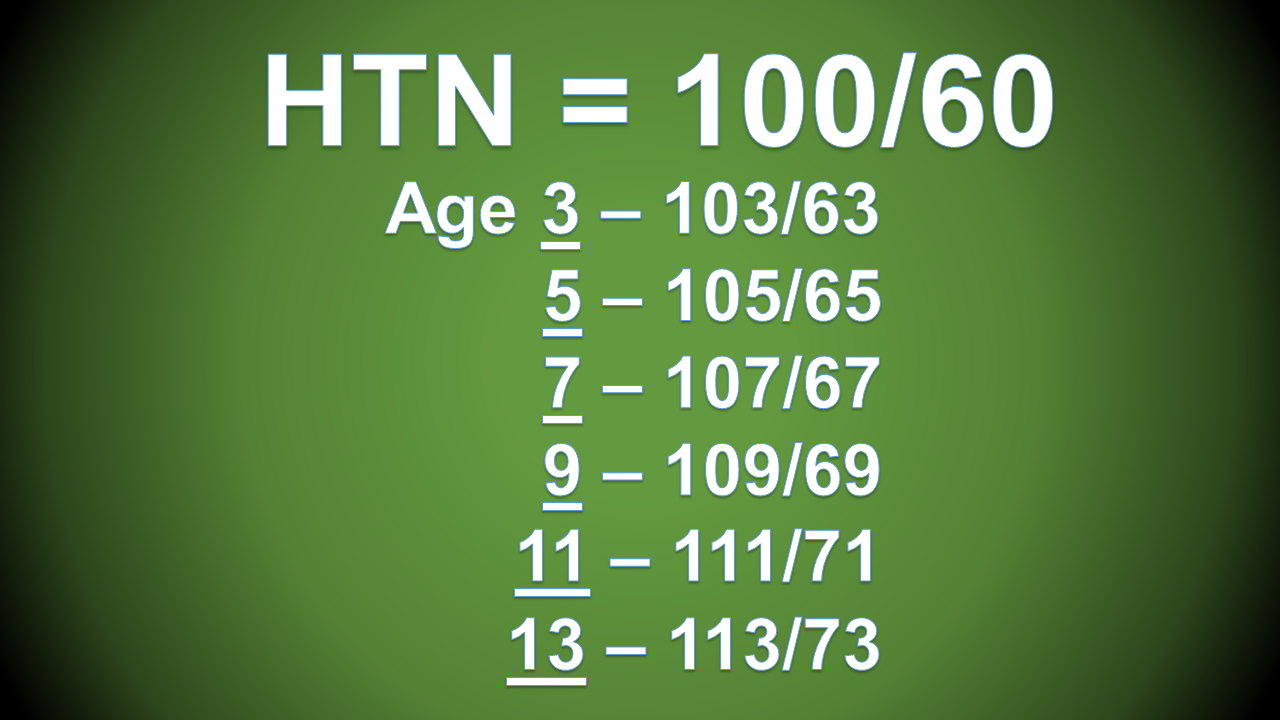
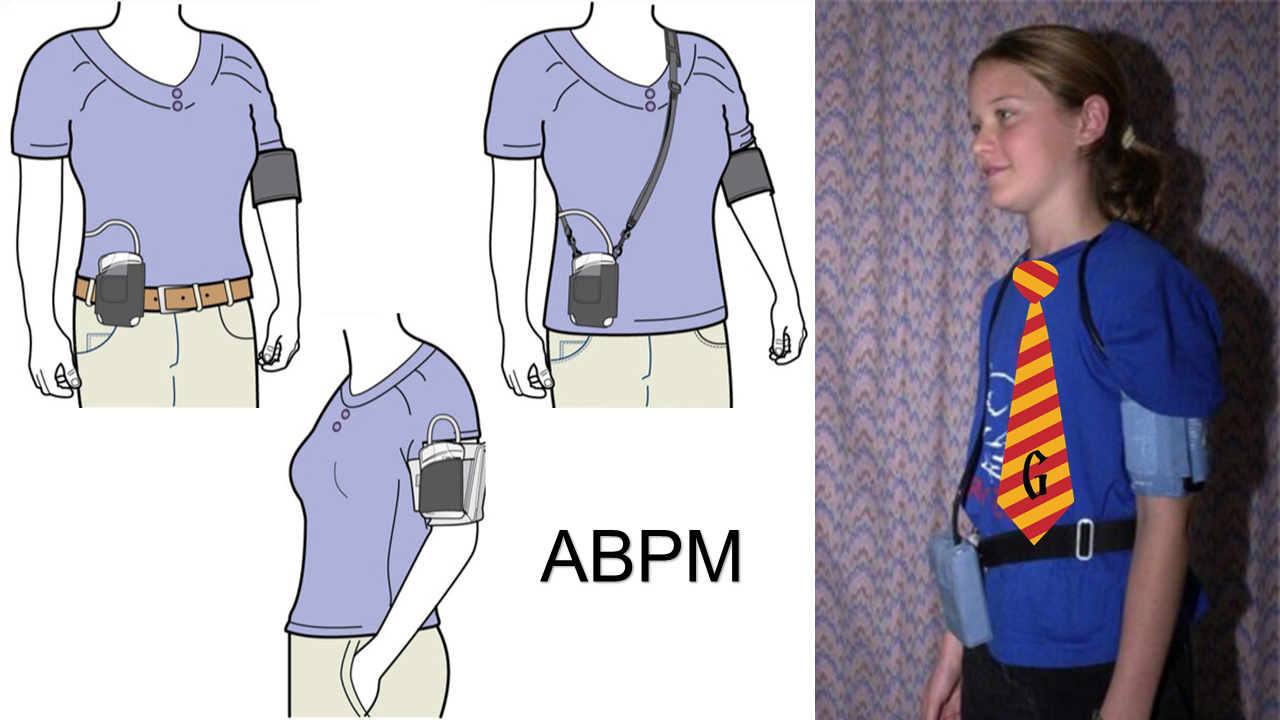
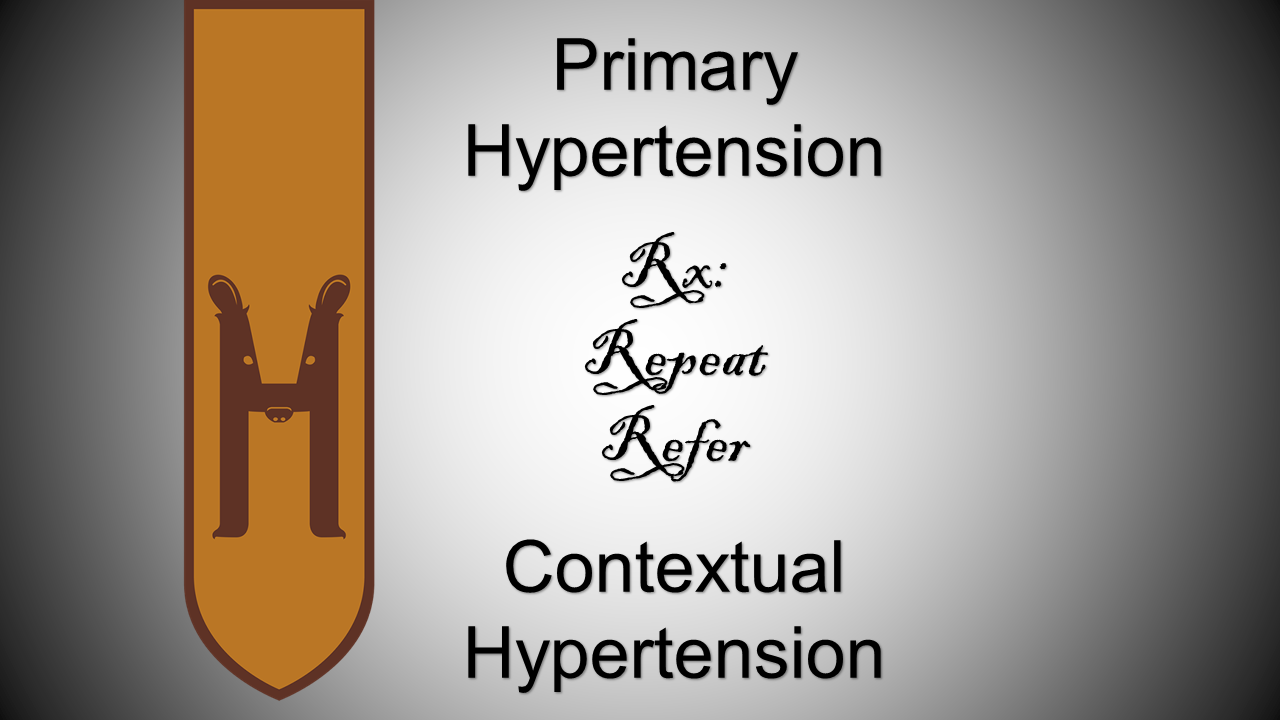
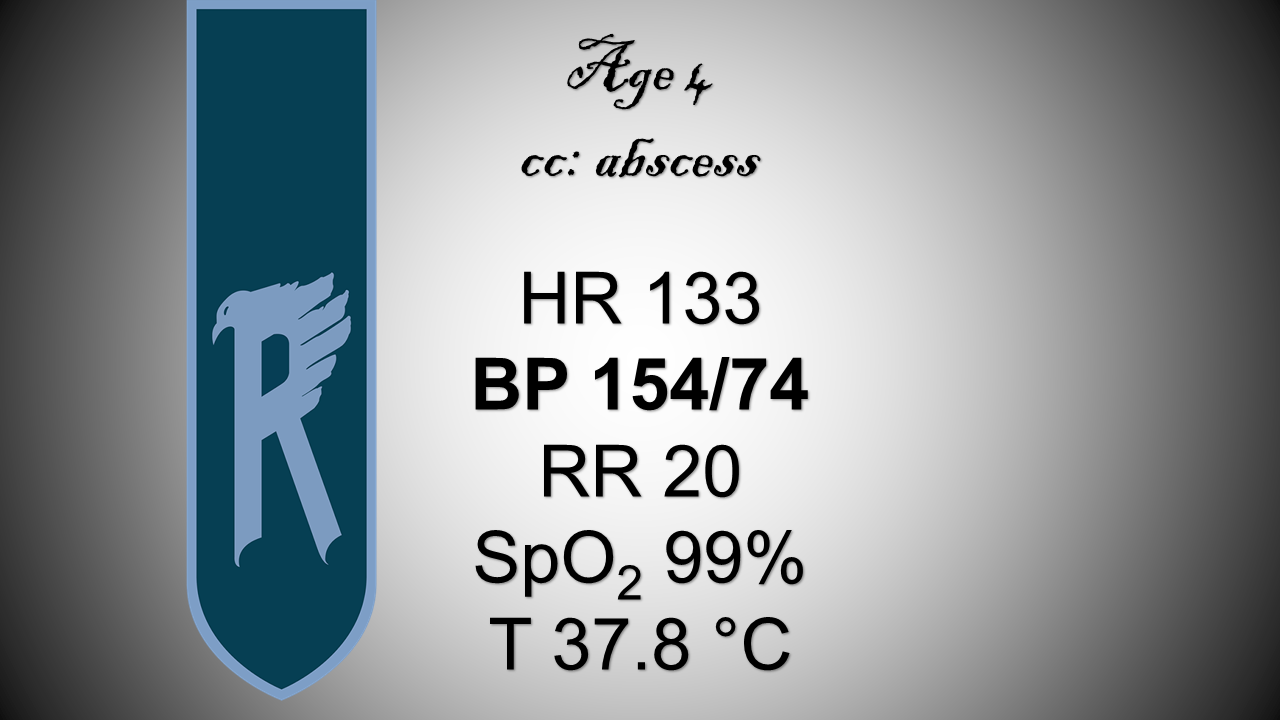
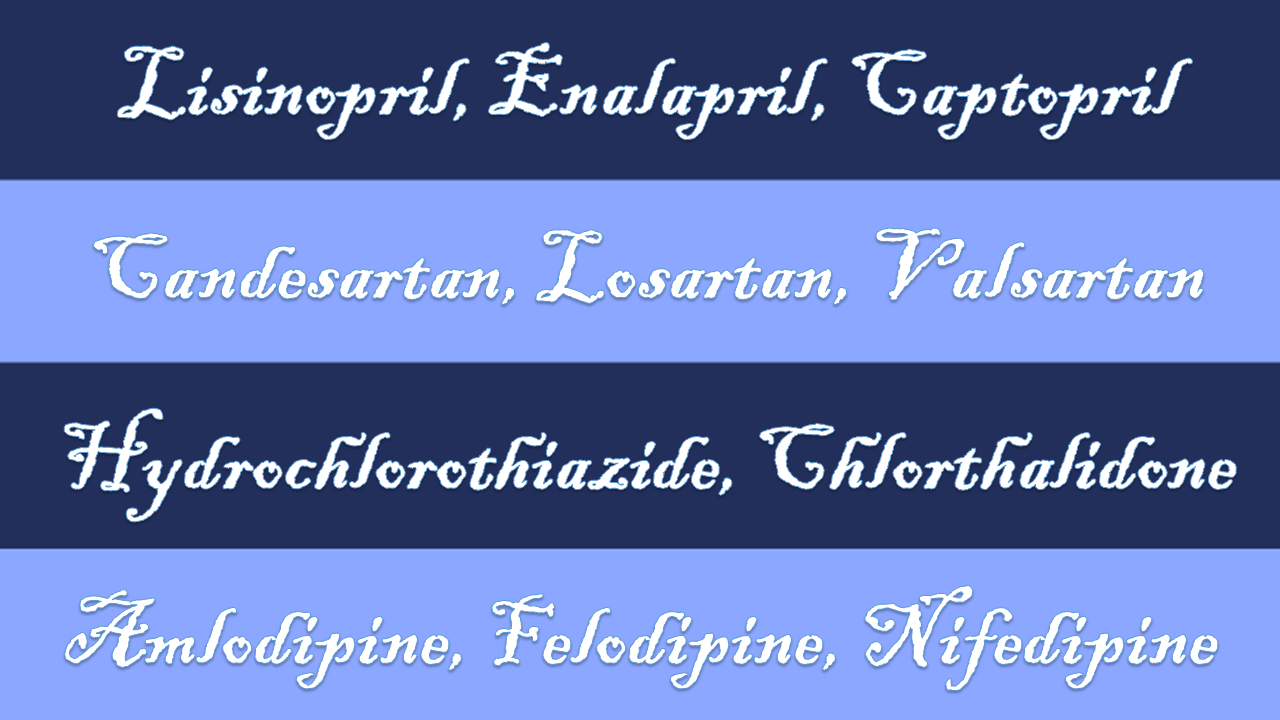
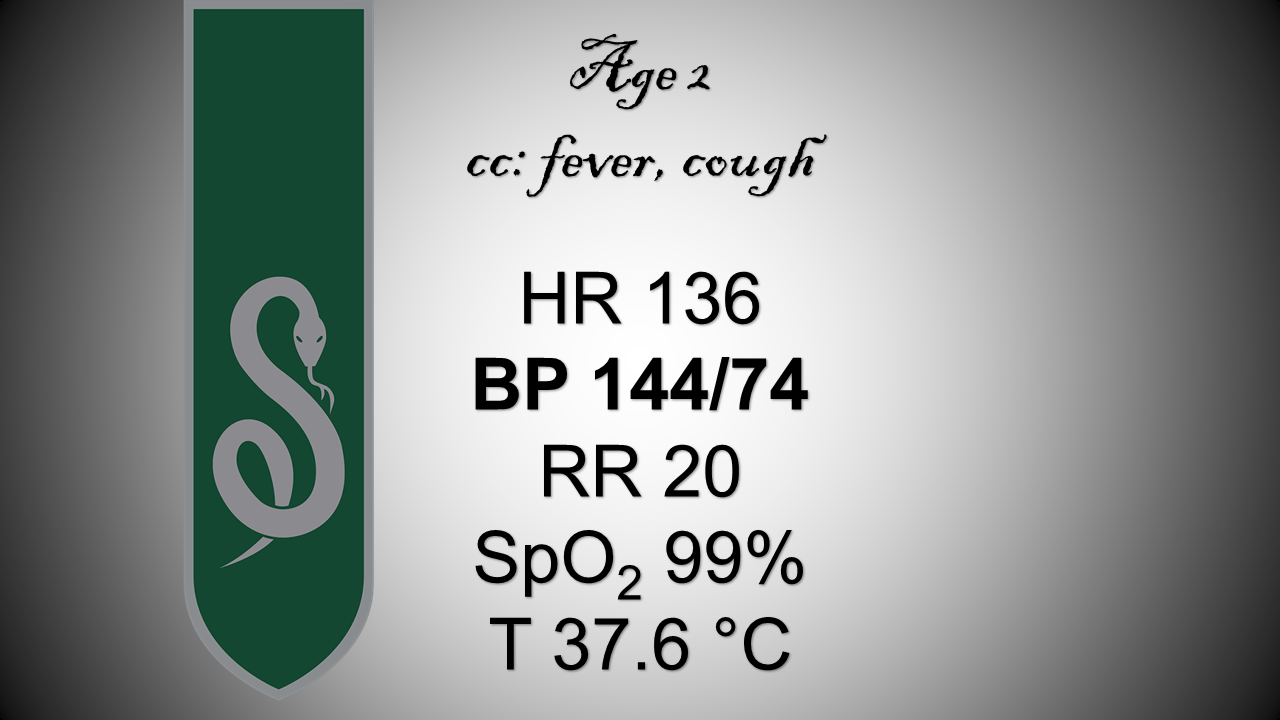
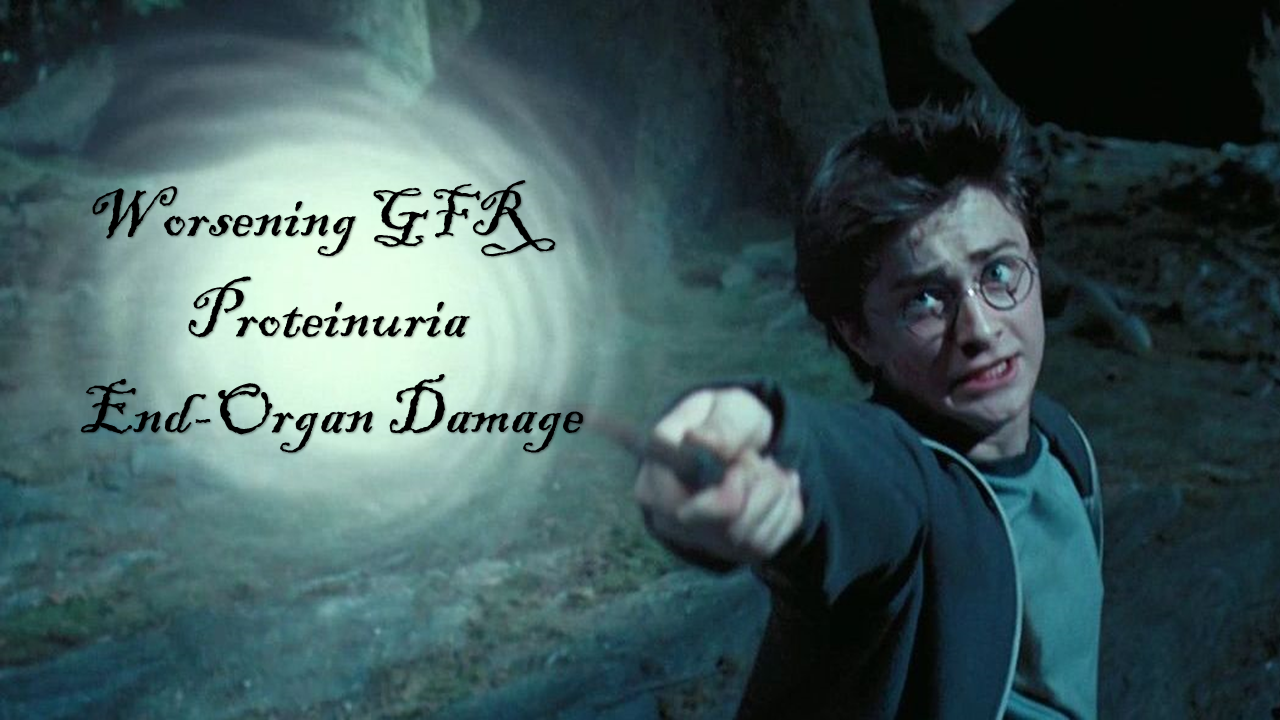
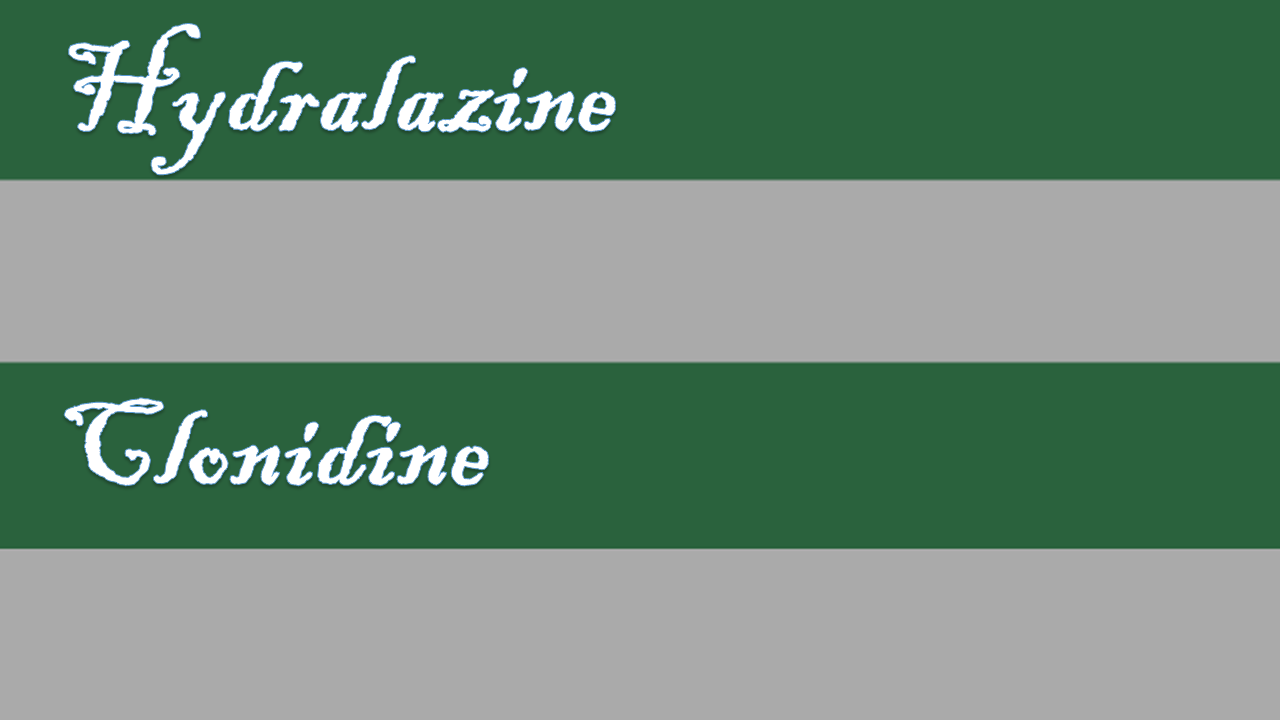
Baracco R et al. Pediatric Hypertensive Emergencies. Curr Hypertens Rep. 2014; 16:456.
Belsha CW. Pediatric Hypertension in the Emergency Department. Ann Emerg Med. 2008; 51(3):21-24.
Chandar J et al. Hypertensive crisis in children. Pediatr Nephrol. 2012; 27:741-751.
Dionne JM et al. Hypertension Canada’s 2017 Guidelines for the Diagnosis, Assessment, Prevention, and Treatment of Pediatric Hypertension. Canadian J Cardiol. 2017; 33:577-585
*Flynn JT, Kaelber DC, Baker-Smith CM, et al; SUBCOMMITTEE ON SCREENING AND MANAGEMENT OF HIGH BLOOD PRESSURE IN CHILDREN. Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents. Pediatrics. 2017; 140(3):e20171904
Gilhotra Y et al. Blood pressure measurements on children in the emergency department. Emergency Medicine Australasia. 2006; 18:148-154.
Lurbe E et al. 2016 European Society of Hypertension guidelines for the management of high blood pressure in children and adolescents. J Hypertens. 2016; 34:1-35.
Patel NH et al. Evaluation and management of pediatric hypertensive crises: hypertensive urgency and hypertensive emergencies. Open Access Emergency Medicine. 2012; 4:85-92.
Yang WC et al. Clinical Analysis of Hypertension in Children Admitted to the Emergency Department. Pediatr Neonatol. 2010; 1:44-51.
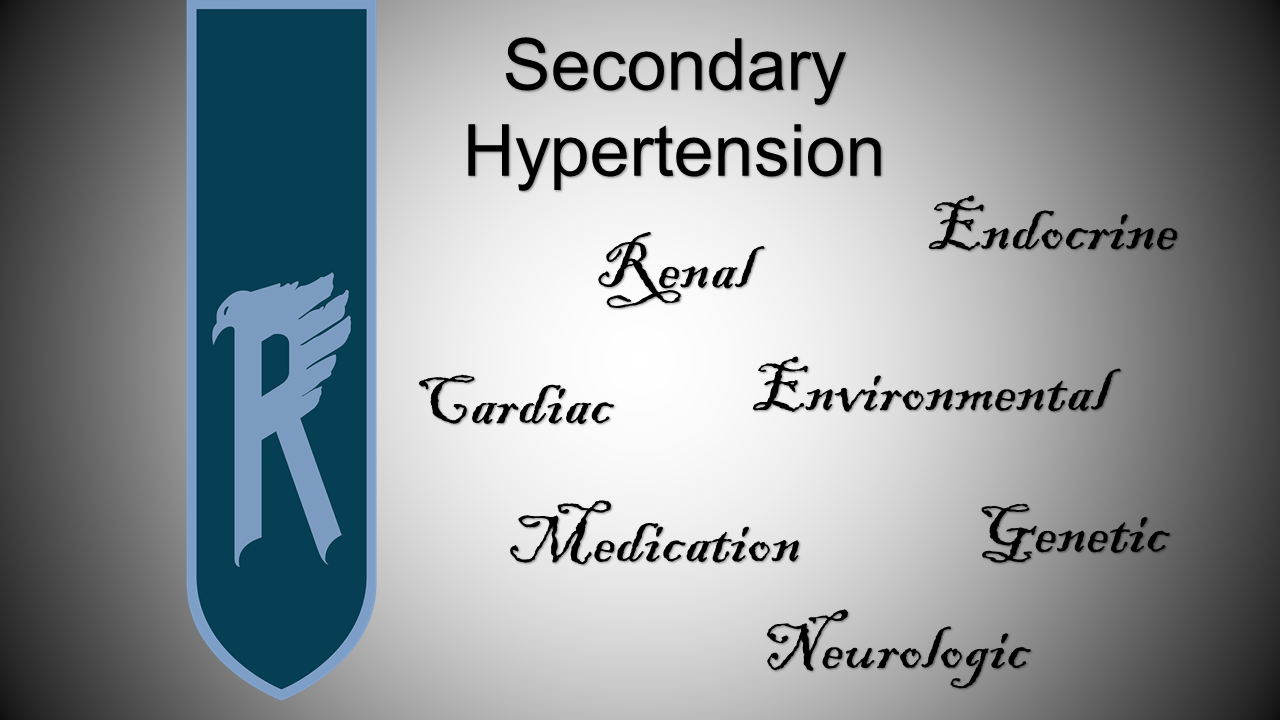
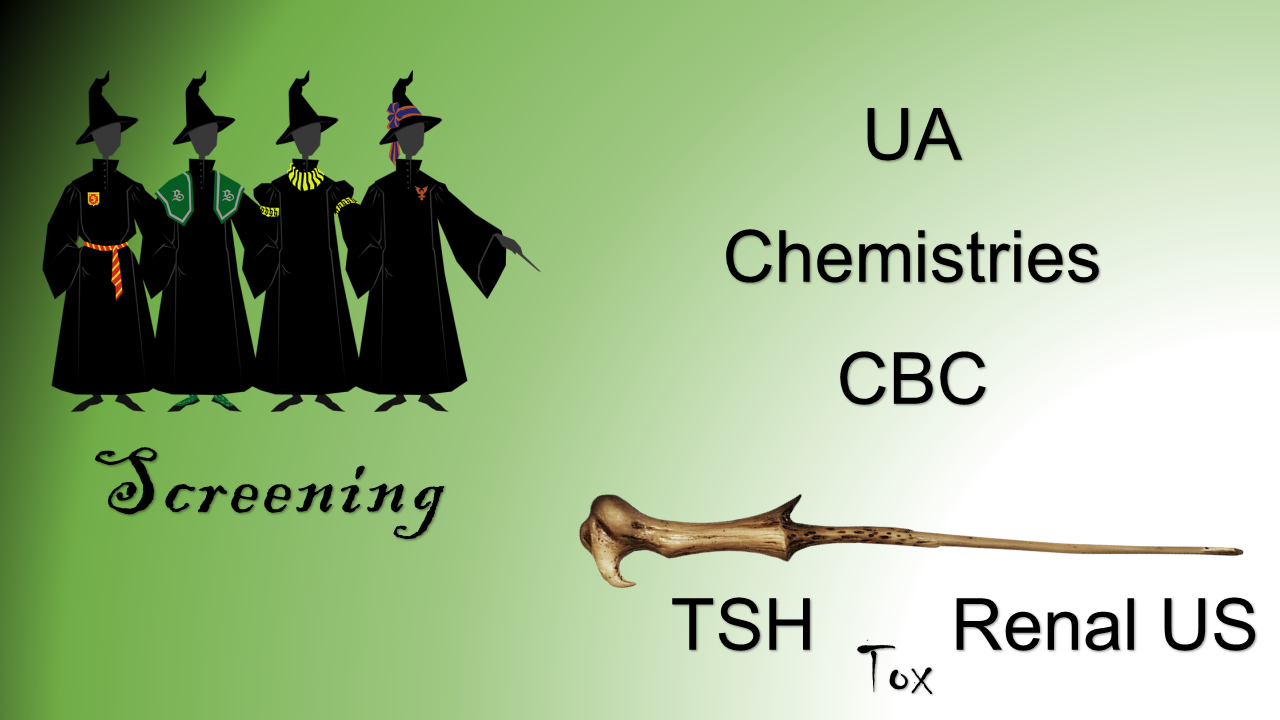
Addendum: Causes of Malignant Hypertension by Age
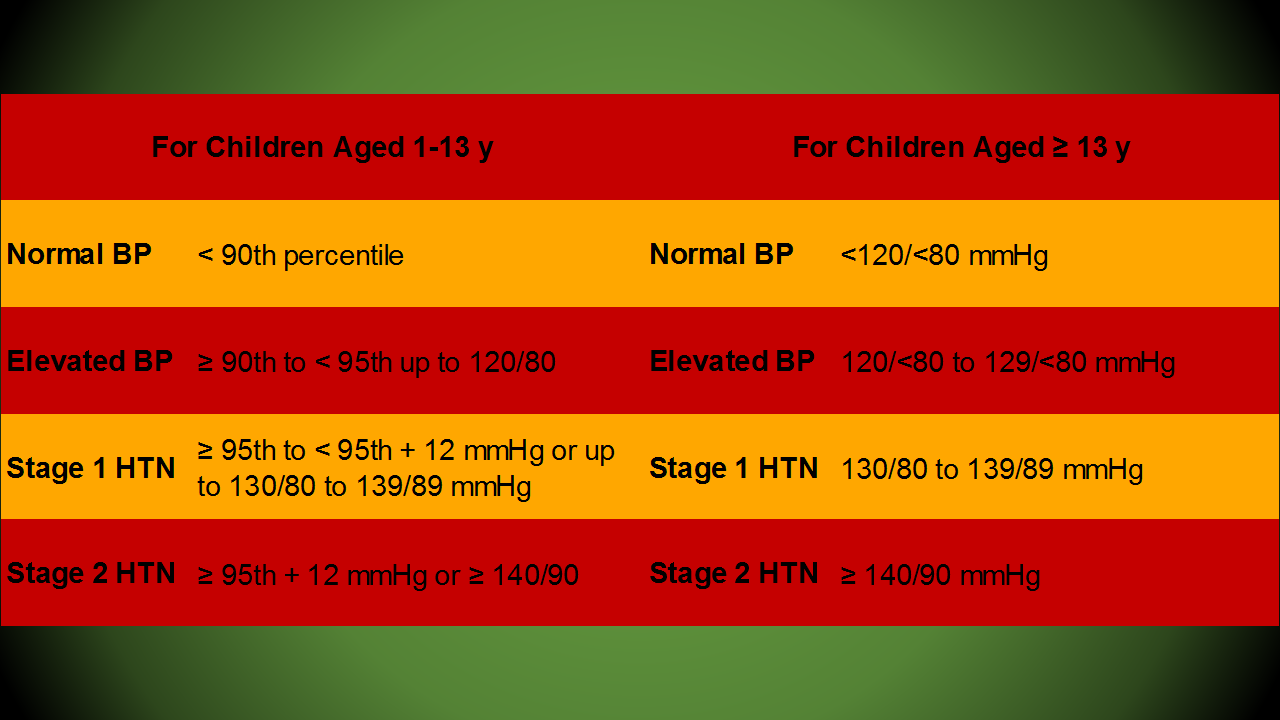
| Infant to Toddler | Preschool to School Age | Adolescent to Adult |
| Renal disease | Renal disease | Primary hypertension |
| Coarctation of the aorta | Coarctation of the aorta | Medication non-adherence |
| Bronchopulmonary dysplasia | Drug induced/toxicologic | Renal disease |
| Increased intracranial pressure | Increased intracranial pressure | Increased intracranial pressure |
| Volume overload | Pheochromocytoma | Pheochromocytoma |
| Congenital adrenal hyperplasia | Primary hypertension | Drug induced/toxicologic |
Adapted from: Constantine E. Hypertension. In: Textbook of Pediatric Emergency Medicine, 6th Ed. Fleischer GR, Ludwig S, Henretig FM (Eds). Lippincott, Williams & Wilkins, Philadelphia. 2010; p315.
This post and podcast are dedicated to Manpreet 'Manny' Singh for his collegiality, collaboration, and overall awesomeness.
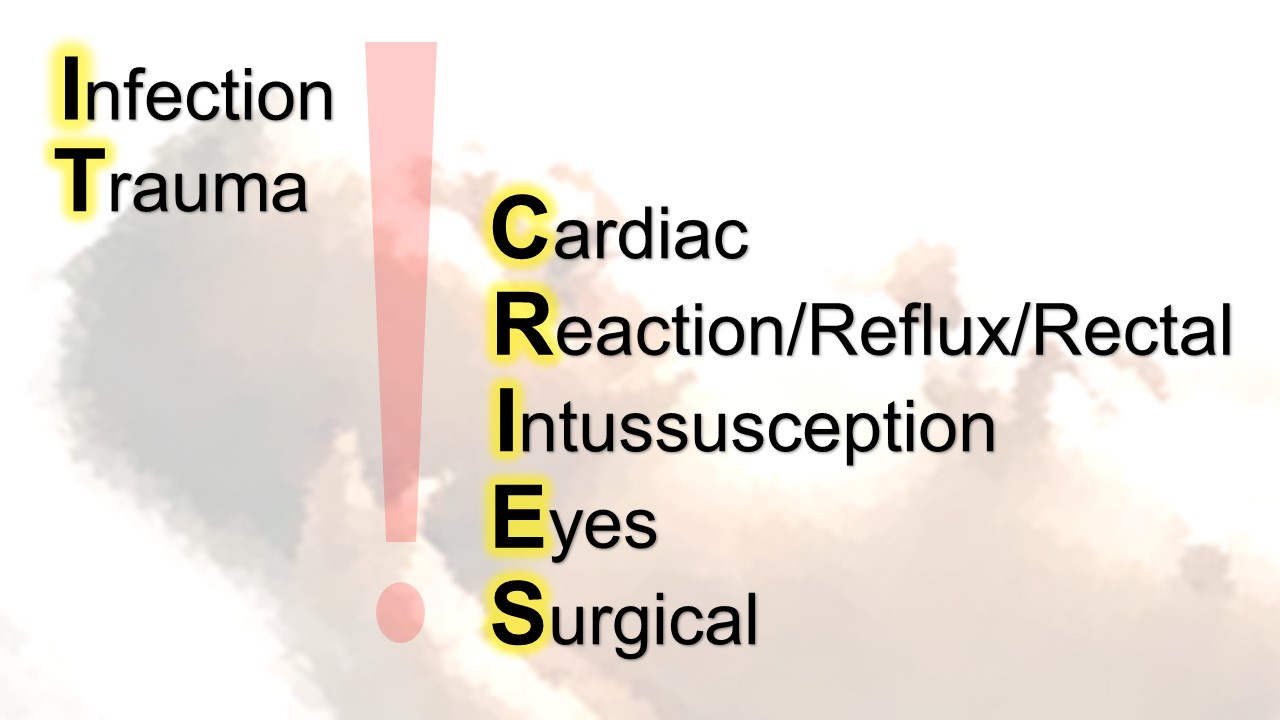
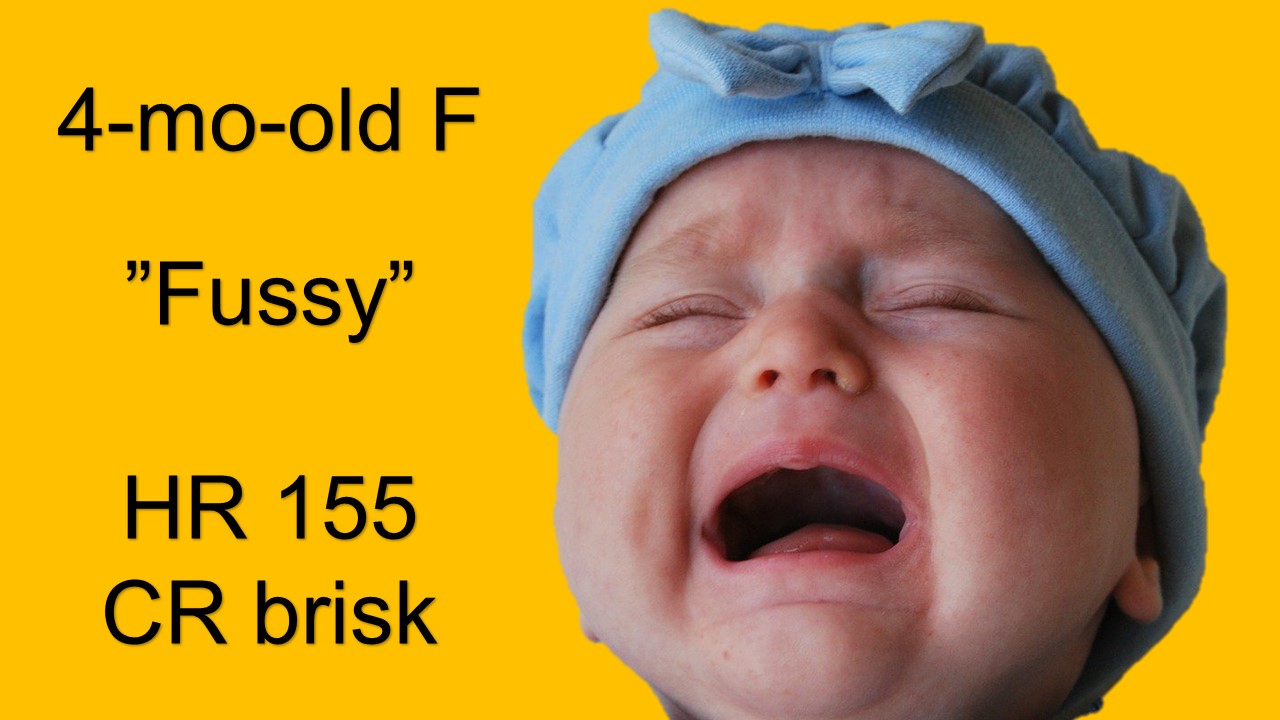
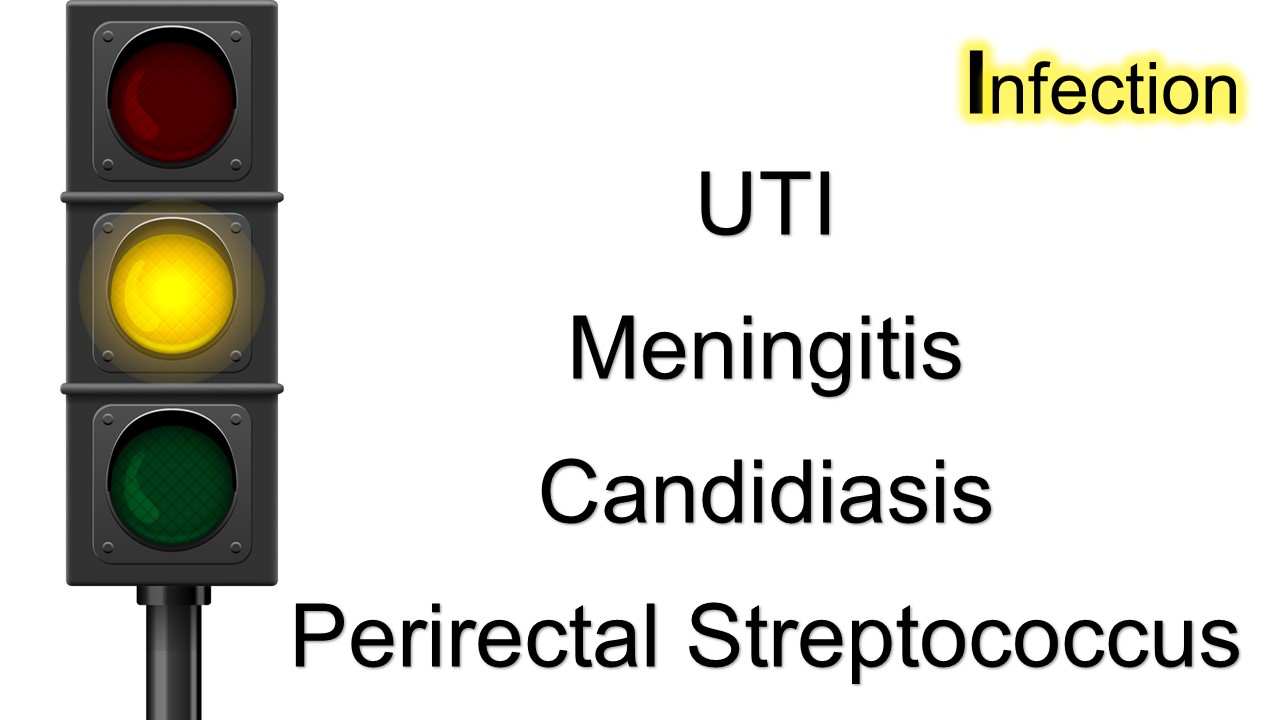
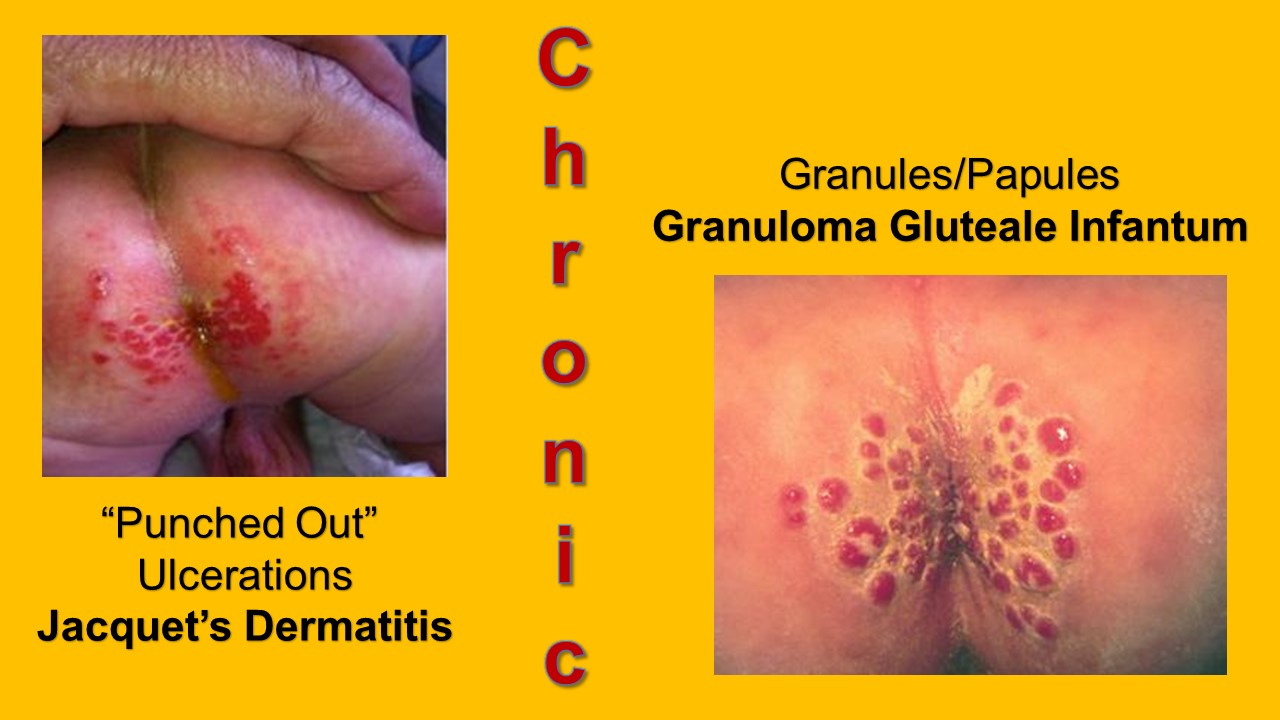
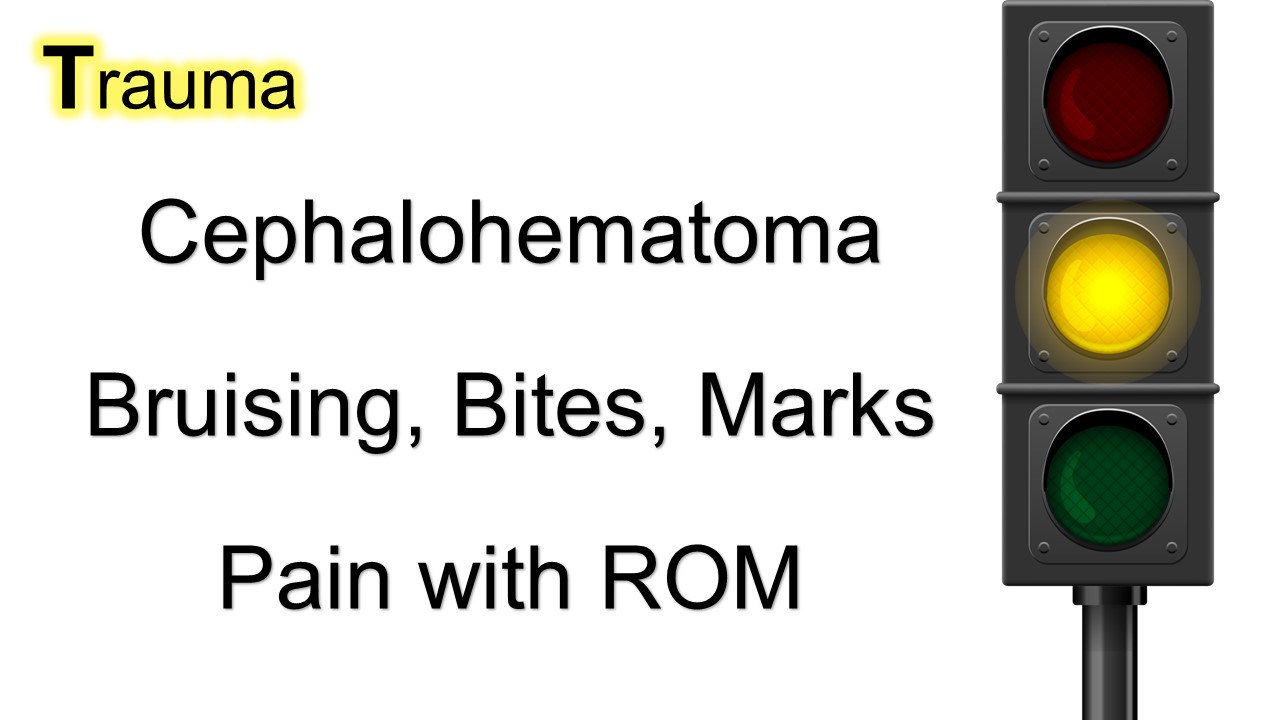
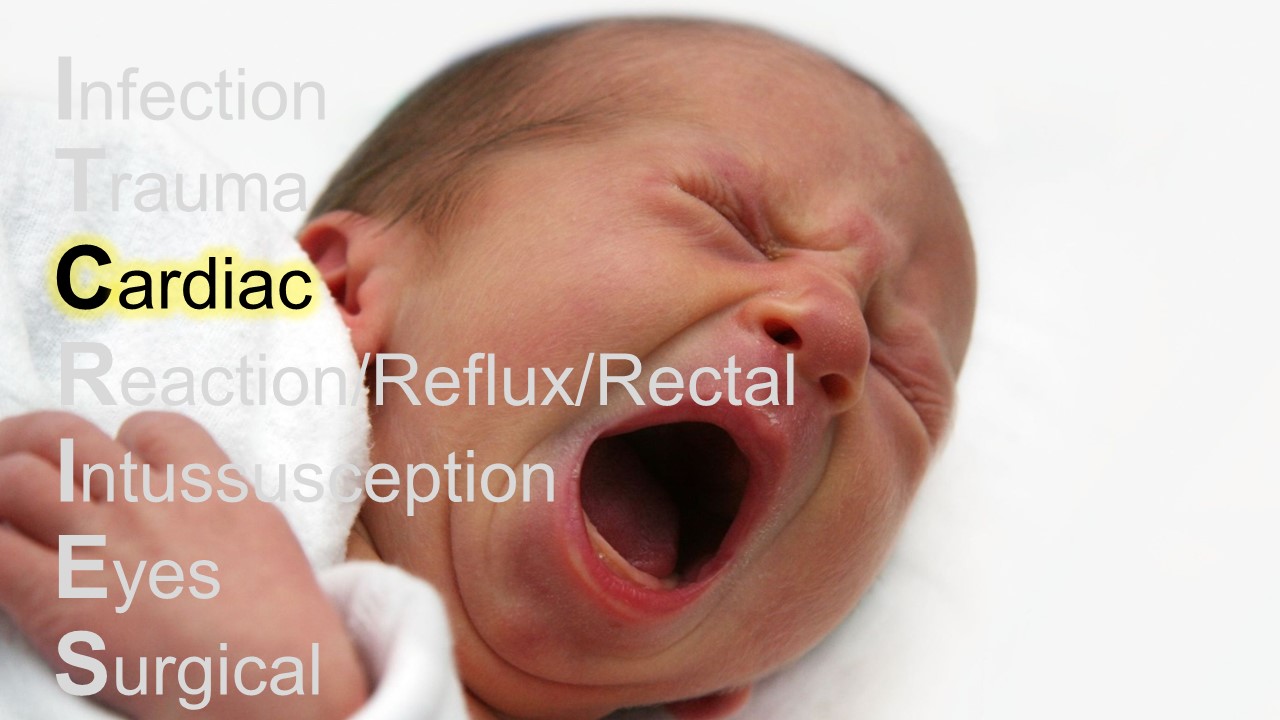
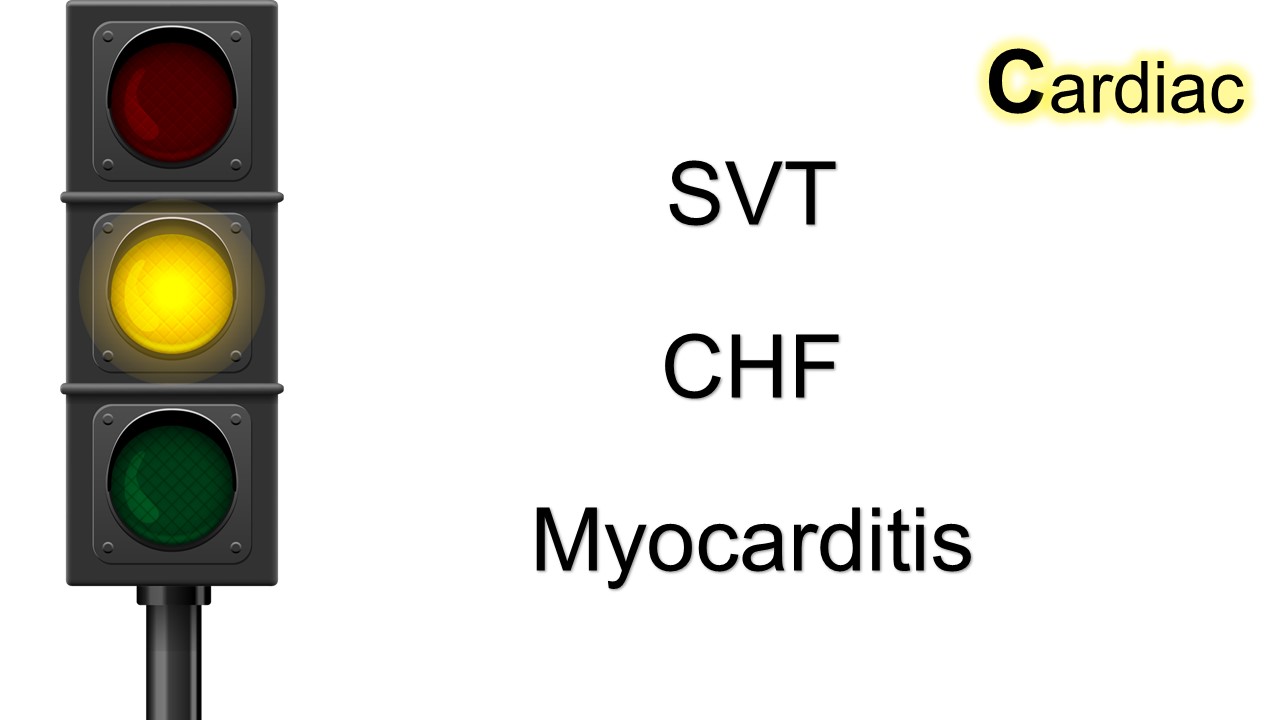
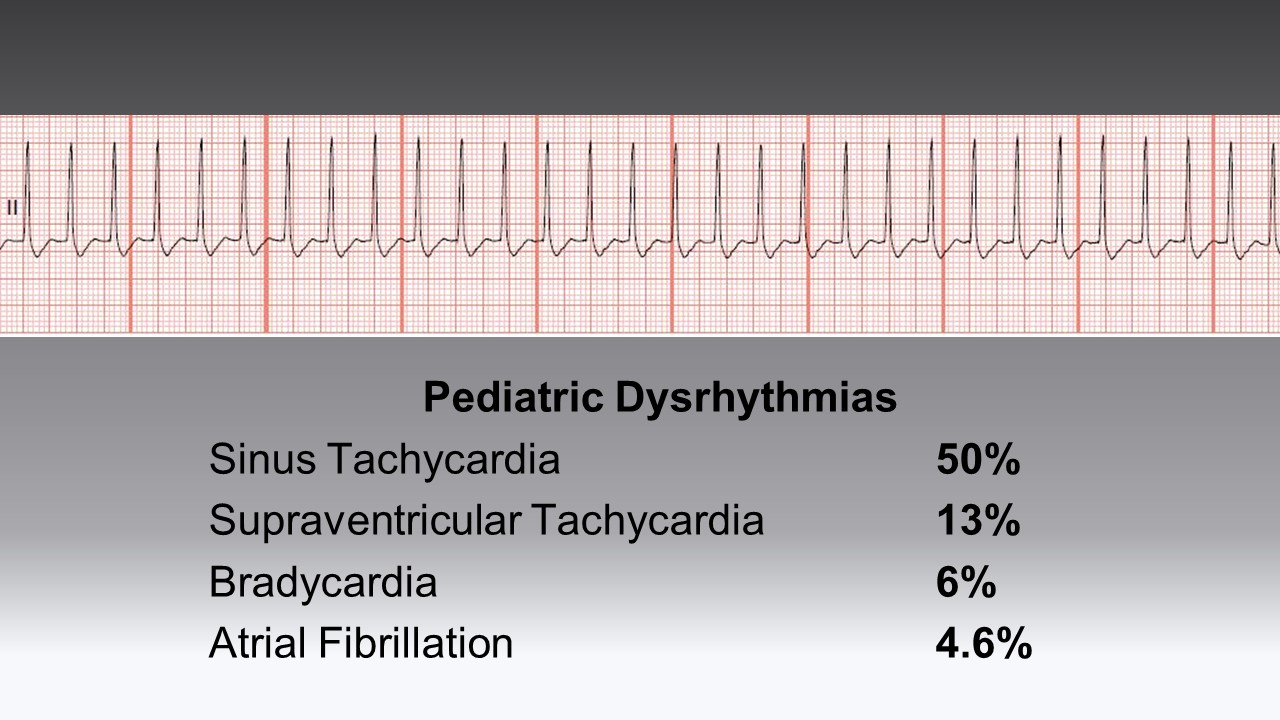
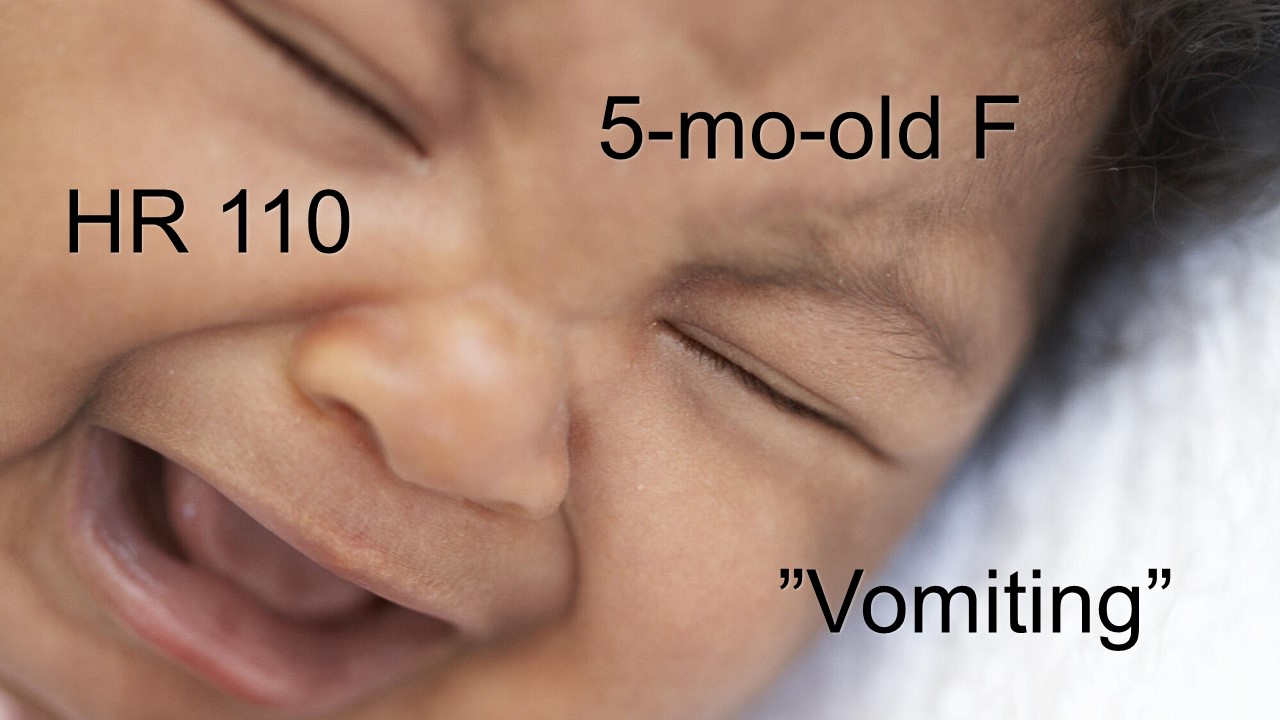
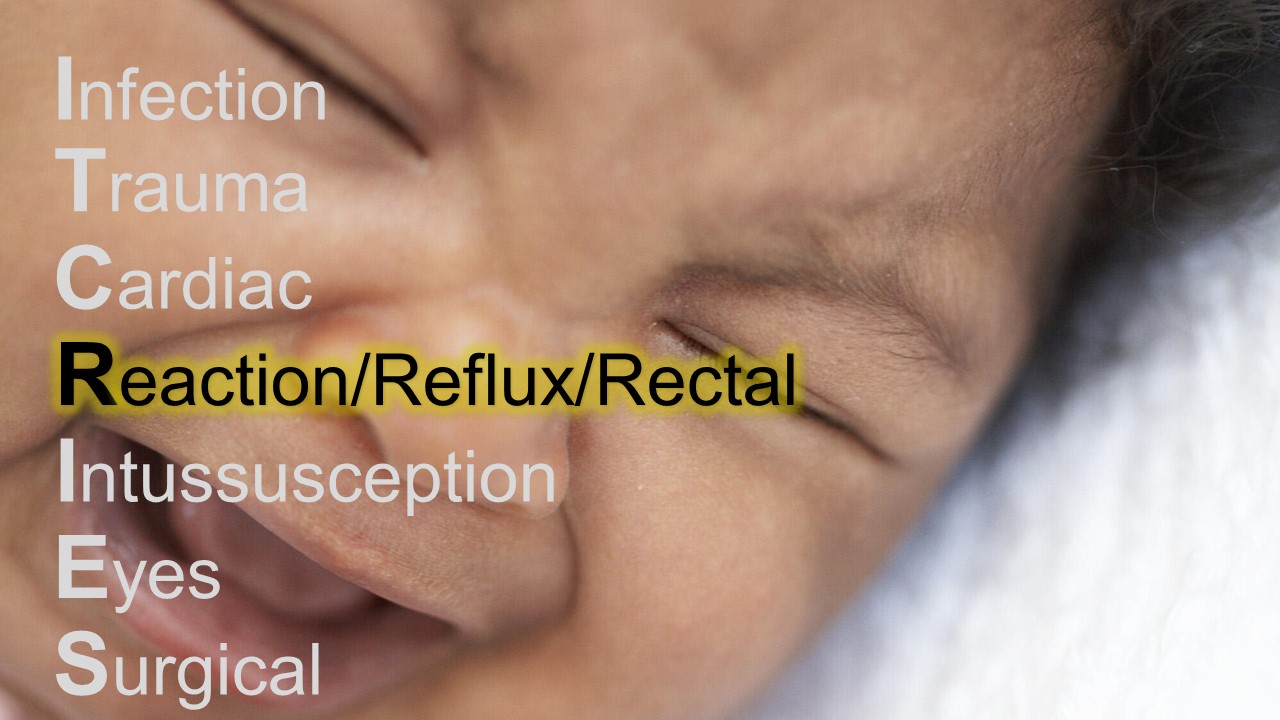
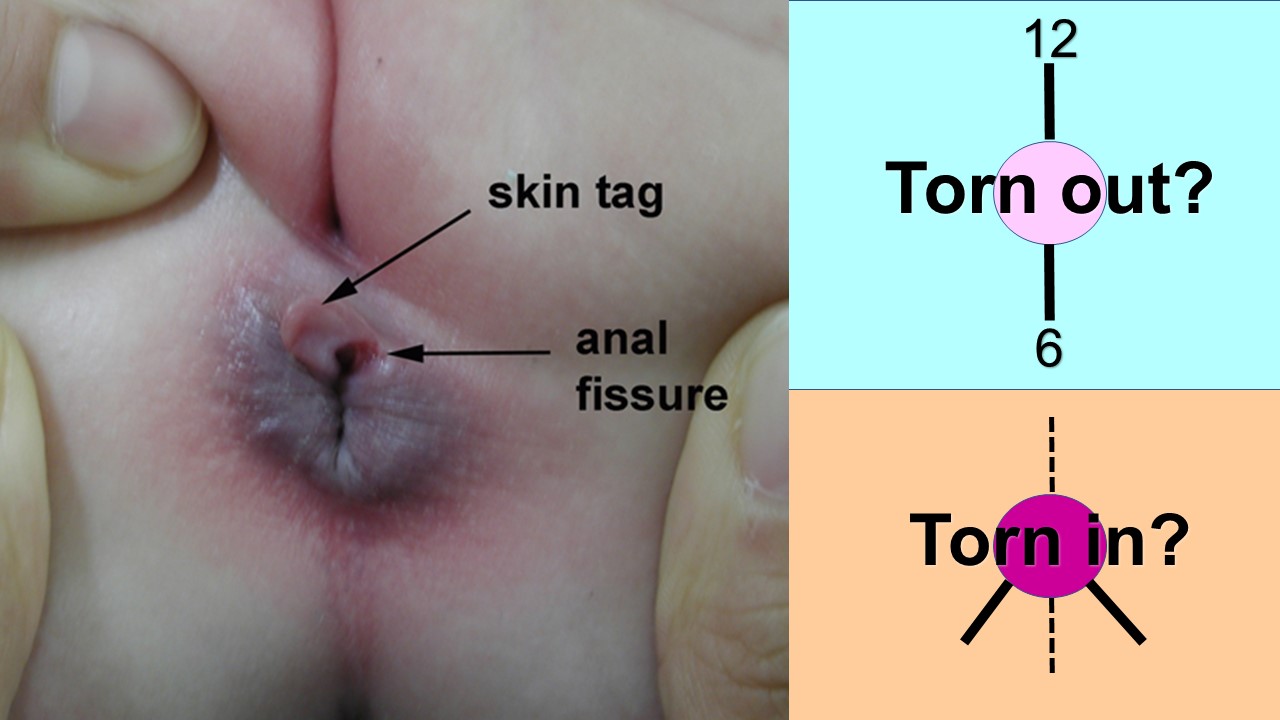
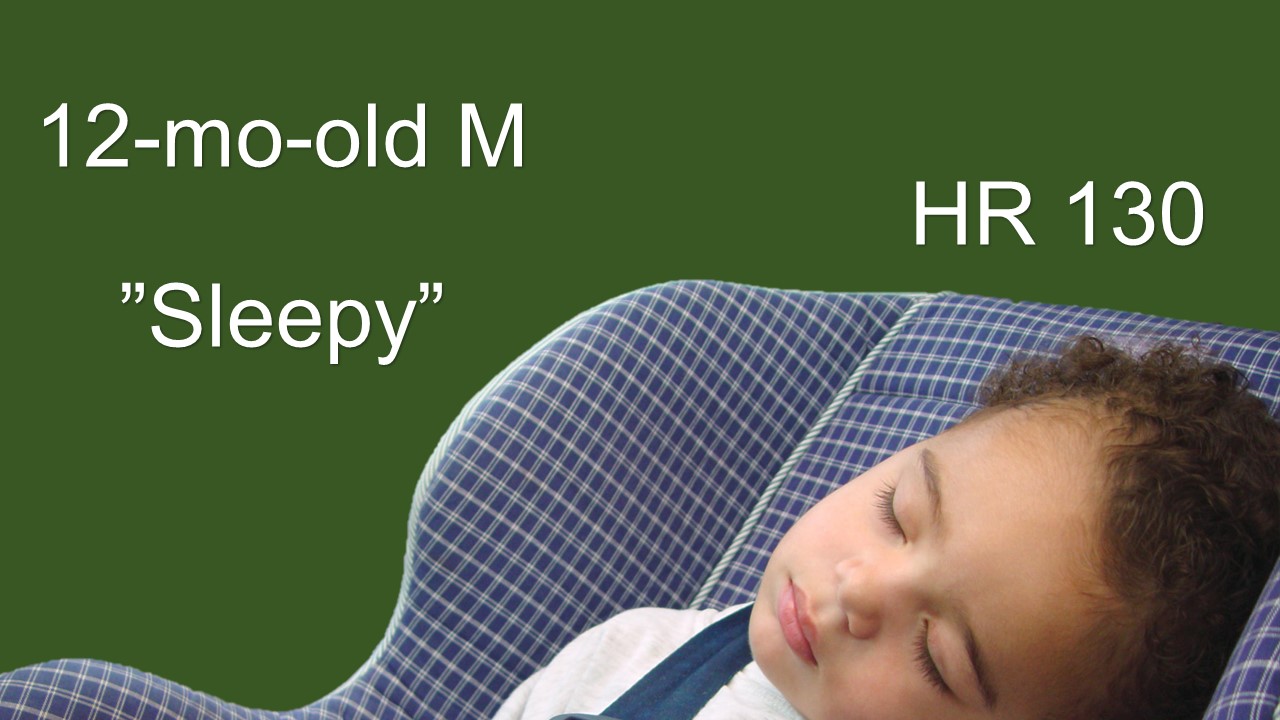
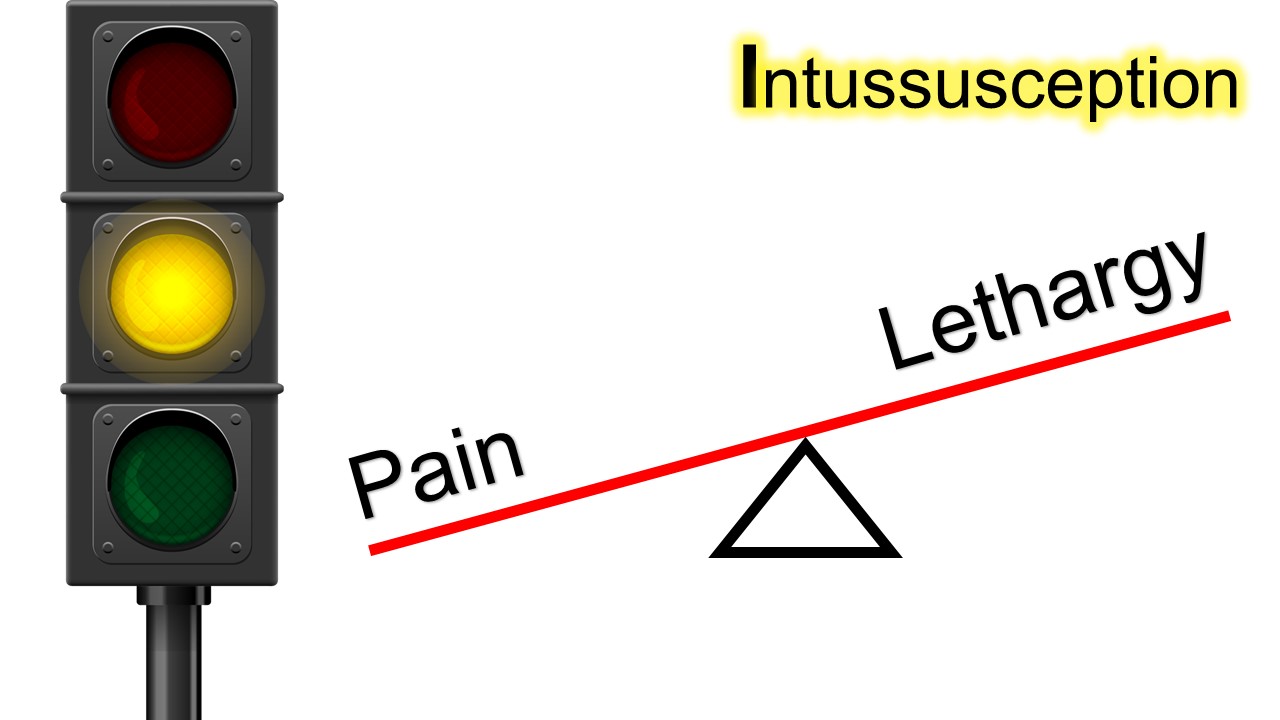
A Social Visit or Your Most Dangerous Presentation Tonight?
[Details in Audio]
This post and podcast are dedicated to Henry Goldstein, B.Pharm, MBBS for his tireless dedication to all things #FOAMed, #FOAMped, and #MedEd. You are awesome. Make sure to visit Don't Forget the Bubbles!
References
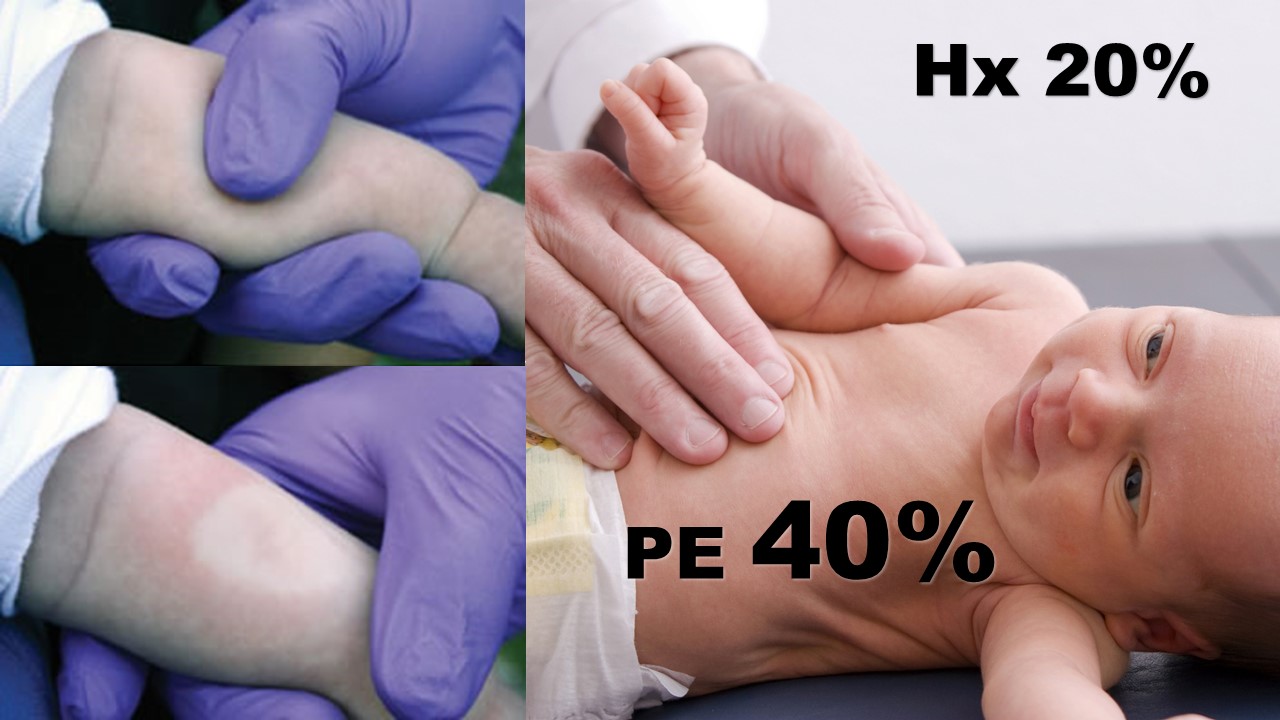
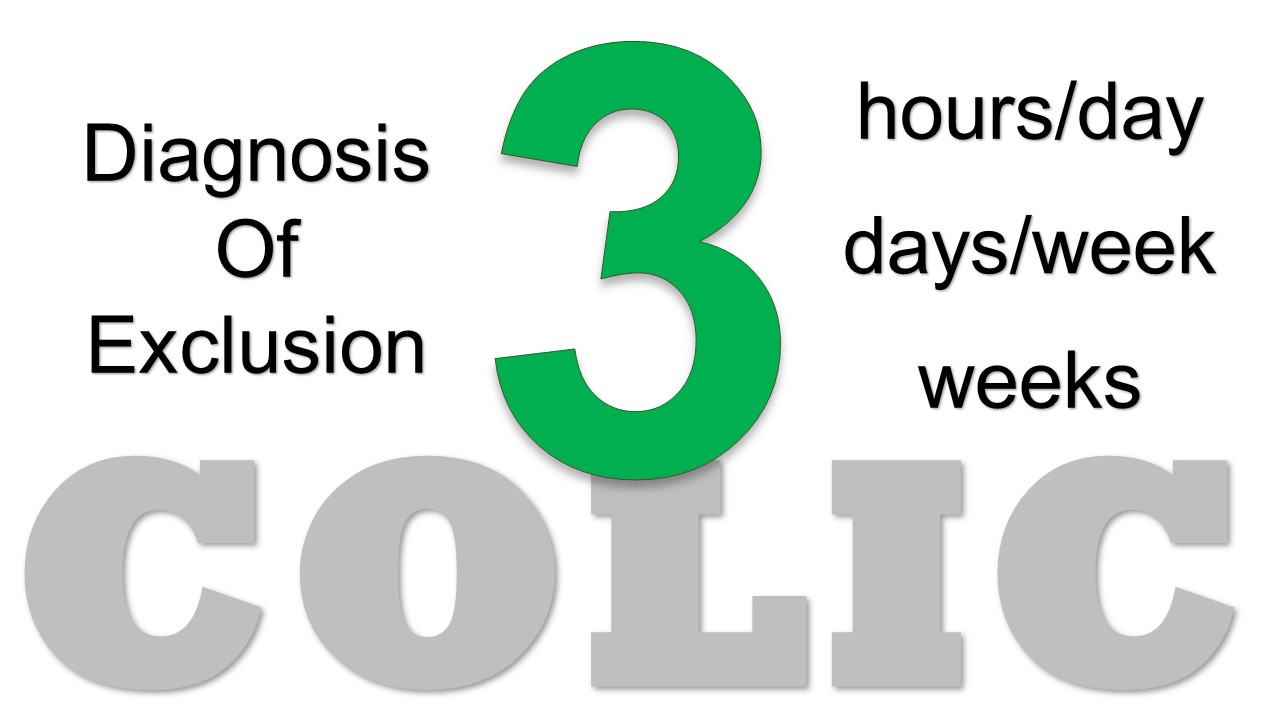
Cohen GM, Albertini LW. Colic. Pediatr Rev. 2012; 33(7):332-3.
Friedman SB et al. The crying infant: diagnostic testing and frequency of serious underlying disease. Pediatrics. 2009; 123(3):841-8
Herman M, Le A. The crying infant. Emerg Med Clin North Am. 2007 Nov;25(4):1137-59.
Poole SR. The infant with acute, unexplained, excessive crying. Pediatrics. 1991; 88 (3): 450-5.
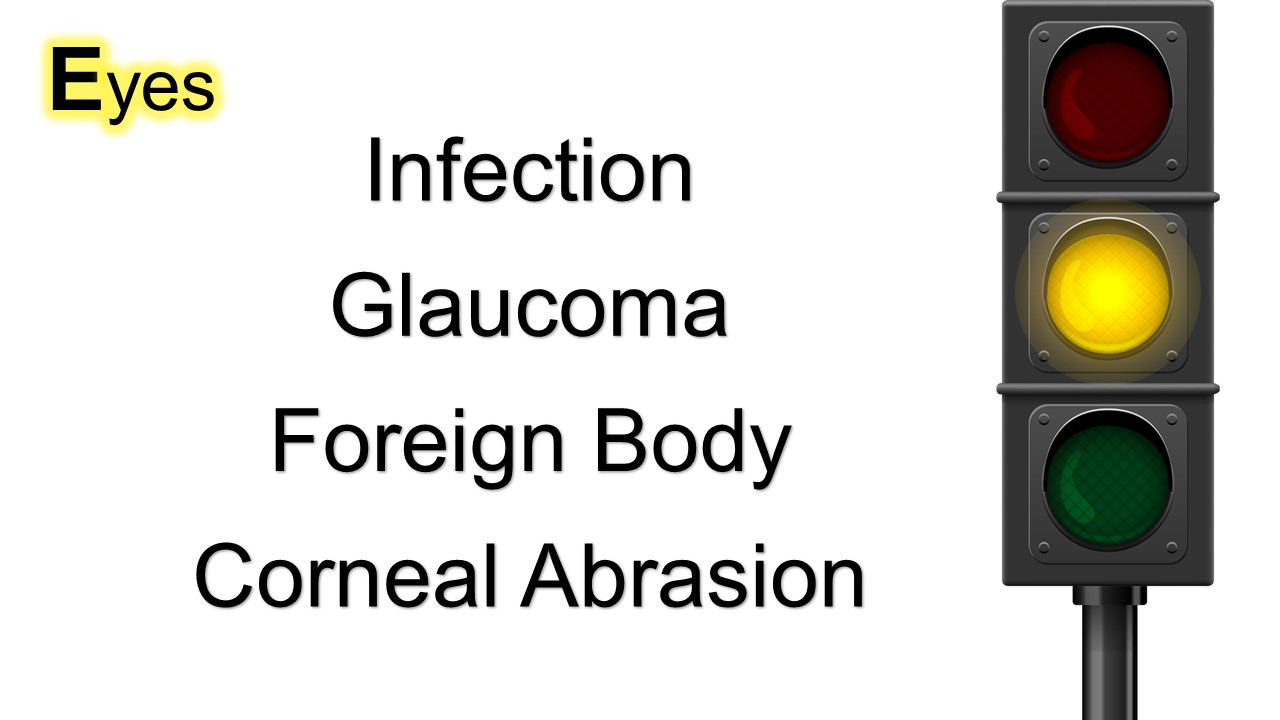
Prentiss KA, Dorfman DH. Pediatric Opthalmology in the Emergency Department. Emerg. Med. Clin. N. Am. 2008; 26: 181-198.
Shope TR, Rieg TS, Kathiria NN. Corneal abrasions in young infants. Pediatrics. 2010 Mar;125(3):e565-9. Epub 2010 Feb 8.
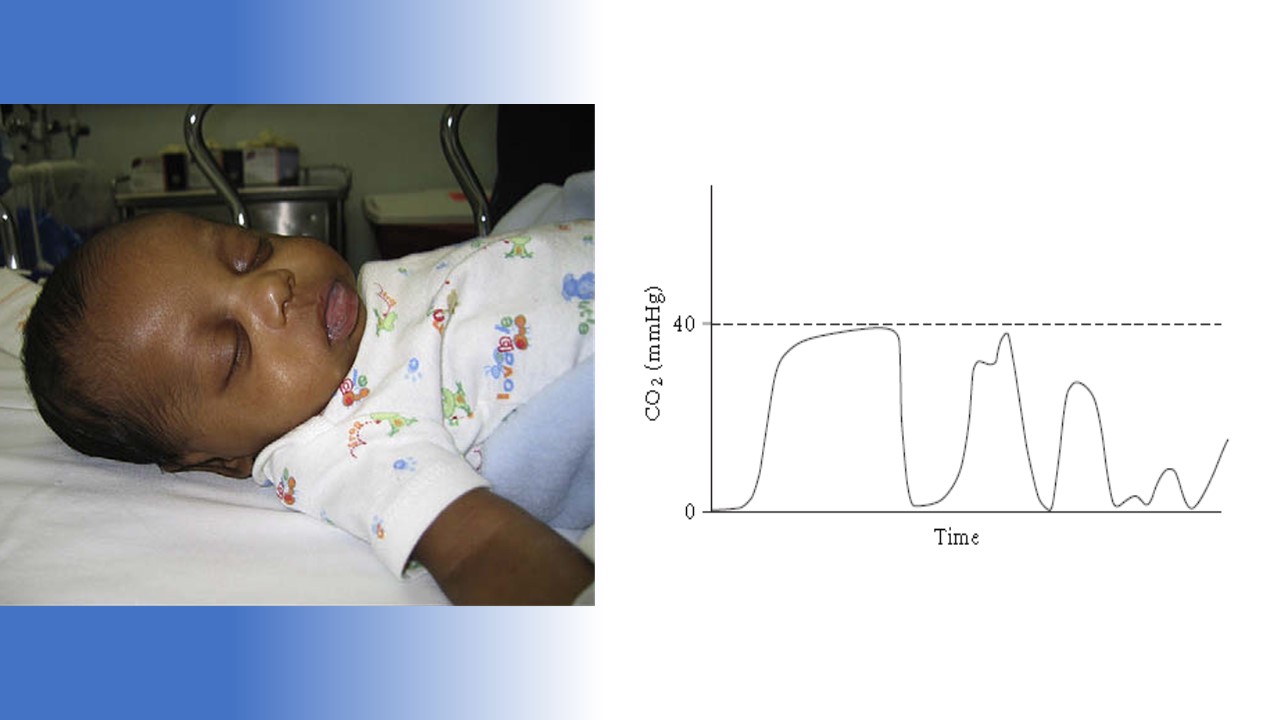
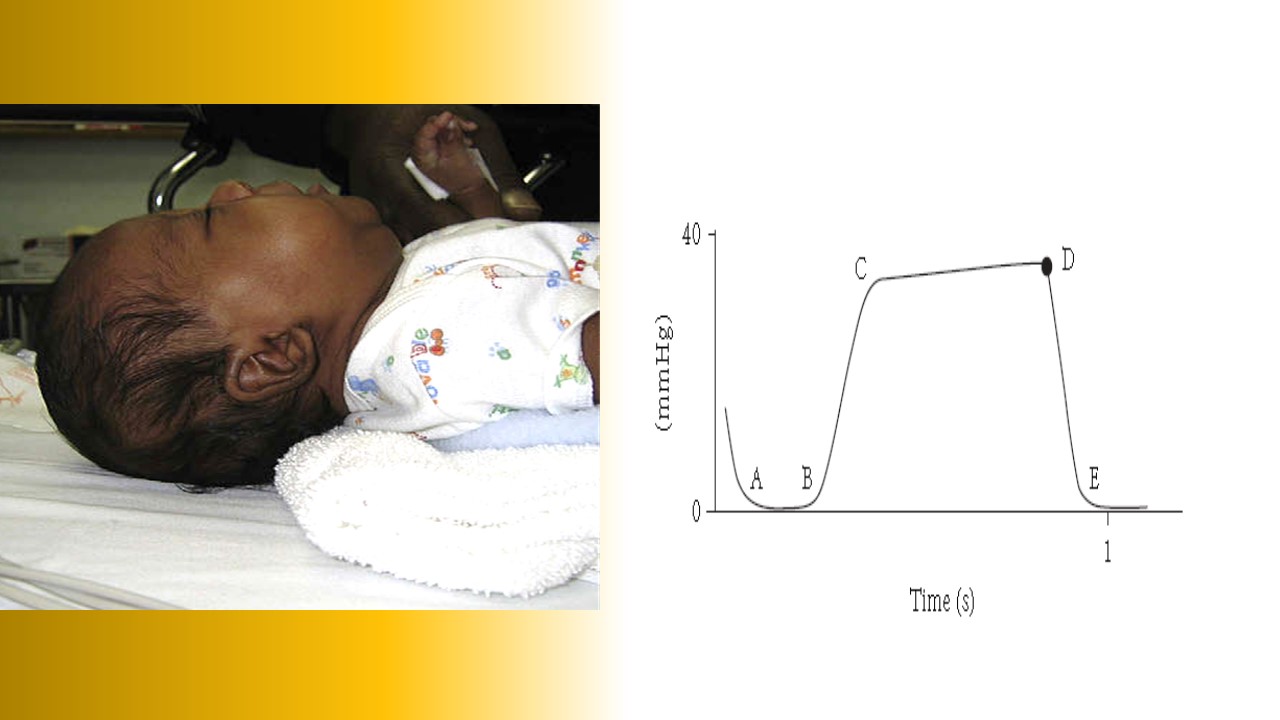
You know how to intubate safely. You can recite all of the Ps backwards and forwards.
Until you can't.
Real-time trouble-shooting.
[Details in Audio]
This post and podcast are dedicated to Mads Astvad for sharing his enthusiasm, clinical excellence, and #FOAMed warrior spirit.
Tak, min ven! #SMACConia #Vikingeblod
Ovarian torsion is like the MI of the pelvis. Sometimes all it takes is a good story to investigate.
When to worry, when to walk it off, and when to work it up:
What is the typical presentation of ovarian torsion?
There is none. The presentation varies so much, we need a rule to live by:
Unilateral pelvic pain in a girl is ovarian torsion until proven otherwise. This includes the cases in which you are concerned about appendicitis. They both can be fake-outs.
Often the pain is severe and abrupt, but trying to tease this out is often not fruitful.
Here are the often-reported signs and symptoms associated with ovarian torsion:
Stabbing pain, 70%
Nausea and vomiting, 70%
Sudden, sharp pain in the lower abdomen, 59%
Pain radiating to the back, flank, or groin, 51%
Peritoneal signs, 3%
Fever, less than 2%
And of course…no pain on presentation…30%...intermittent torsion.
What is the mechanism of ovarian torsion?
- Structurally abnormal ovary (including cysts) that causes the ovary to flop over and twist on its vascular axis
- Hypermobile ovary with vigorous movement twists on its vascular pedicle and cuts off blood supply
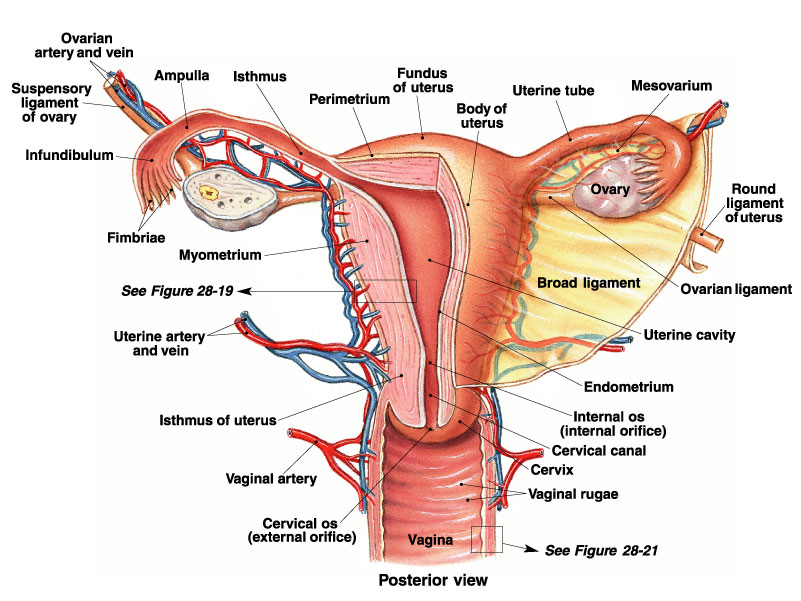
The Dual Blood Supply to the Ovaries: Why Doppler Flow can Fool You
What ultrasound findings suggest ovarian torsion?
- The enlarged hyper or hypoechoic ovary from generalized edema
- Peripherally displaced follicles with hyperechoic central stroma – this is called the string of pearls sign, because the stroma is edematous, leaving the follicles to stand out
- A midline ovary – if the ovary magically makes it to midline, something is up
- Free fluid in the pelvis – this is seen in the vast majority of cases
As far as Doppler flow goes, you may see one of several scenarios:
- Little or no venous flow – this is very common, as we talked about, because the low pressure venous system is the first to take a hit in torsion
- Totally absent arterial flow – this is not as common, but totally diagnostic
- There may be no flow in diastole, or the flow may even be reversed. Rememver the red and blue of dopple does not correspond to arterial and venous. Doppler is a vector. Red is fluid coming towards the probe, blue is programmed to present flow away from the probe. If you have just one or the other, then by definition there is a problem with the vascular circuit.
Other things you may see on ultrasound include focal tenderness with the probe, or the whirlpool sign – this is a twisted vascular pedicle.
In children, is there an ovarian size (volume) that rules out torsion?”
In the Journal of Pediatric Radiology, Servaes et al catalogued the ultrasound findings in children with surgically confirmed torsion over a 12 year period. In this case series of 41 patients, the median age was 11. The age range was one month old to 21 years of age. They found that in torsed ovaries, the ovarian volume was 12 x that compared to the normal, non-torsed contralateral ovary.
That is to say, in this case series all torsed ovaries were larger than the normal contralateral ovary.
Summary
Sudden unilateral lower abdominal or pelvic pain in a female? Think torsion.
Have a low threshold for investigation.
Know the performance characteristics of ultrasound findings and involve a gynecologist early.
This post and podcast are dedicated to Stephanie Doniger, MD for her enthusiasm, spirit, and expertise in #MedEd #FOAMed #FOAMped #POCUS
References
Abe M, Sarihan H. Oophoropexy in children with ovarian torsion. Eur. J. Pediatr. Surg. 2004;14:168.
Aziz D, Davis V, Allen L, Langer J. Ovarian torsion in children: Is oophorectomy necessary? J. Pediatr. Surg. 2004;39:750-3.
Bristow RE, Nugent AC, Zahurak ML, et al. Impact of surgeon specialty on ovarian-conserving surgery in young females with an adnexal mass. J. Adolesc. Health 2006;39:411.
Chang YJ, Yan DC, Kong MS, et al. Adnexal torsion in children. Pediatr. Emerg. Care. 2008;24:534-7.
Conforti A, Giorlandino C, Bagolan P. Fetal ovarian cysts management and ovarian prognosis: a report of 82 cases. J. Pediatr. Surg. 2009;44:868; author reply 868-9.
Guthrie BD, Adler MD, Powell EC. Incidence and trends of pediatric ovarian torsion hospitalizations in the United States, 2000-2006. Pediatrics 2010;125:532-8. Epub 2010 Feb 1.
Houry D, Abbott JT. Ovarian torsion: a fifteen-year review. Ann. Emerg. Med. 2001;38:156-9.
Huang TY, Lau BH, Lin LW, Wang TL, Chong CF, Chen CC. Ovarian cyst torsion in a toddler. Am. J. Emerg. Med. 2009;27:632, e1-3.
Hurh PJ, Meyer JS, Shaaban A. Ultrasound of a torsed ovary: characteristic gray-scale appearance despite normal arterial and venous flow on Doppler. Pediatr. Radiol. 2002;32:586-8. Epub 2002 May 25.
Kokoska E, Keller M, Weber T. Acute ovarian torsion in children. Am. J. Surg. 2000;180:462-5.
Oltmann SC, Fischer A, Barber R, Huang R, Hicks B, Garcia N. Cannot exclude torsion – a 15-year review. J. Pediatr. Surg. 2009;44:1212-6; discussion 1217.
Chmitt ER et al. Twist and Shout! Pediatric Ovarian Torsion Clinical Update and Case Discussion. Pediatr Emerg Care. 2013; 29(4):518-523.
Servaes S, Zurakowski D, Laufer MR, Feins N, Chow JS. Sonographic findings of ovarian torsion in children. Pediatr. Radiol. 2007;37:446-51. Epub 2007 Mar 15.
Valsky DV. Added value of the gray-scale whirlpool sign in the diagnosis of adnexal torsion. Ultrasound Obstet. Gynecol. 2010;36:630-4.