Your eyes may fool you...
Keep your differential diagnosis open.

[caption id="attachment_1777" align="alignnone" width="262"]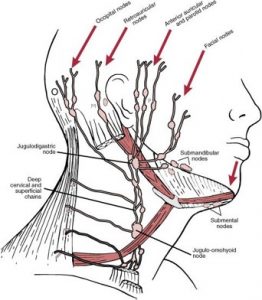 Cervical Node Chain; Lymphadenopathy[/caption] [caption id="attachment_1773" align="alignnone" width="298"]
Cervical Node Chain; Lymphadenopathy[/caption] [caption id="attachment_1773" align="alignnone" width="298"] Bacterial Lymphadenitis[/caption] [caption id="attachment_1772" align="alignnone" width="300"]
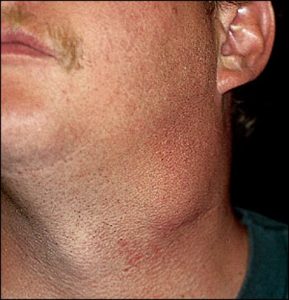
Bacterial Lymphadenitis[/caption] [caption id="attachment_1772" align="alignnone" width="300"]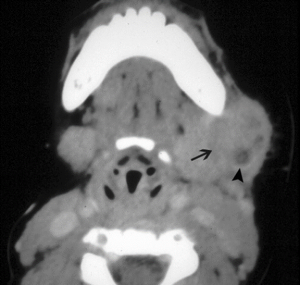 Bacterial lymphadenitis with small abscess[/caption] [caption id="attachment_1771" align="alignnone" width="300"]
Bacterial lymphadenitis with small abscess[/caption] [caption id="attachment_1771" align="alignnone" width="300"] Large Abscess[/caption]
Large Abscess[/caption]

[caption id="attachment_1784" align="alignnone" width="300"]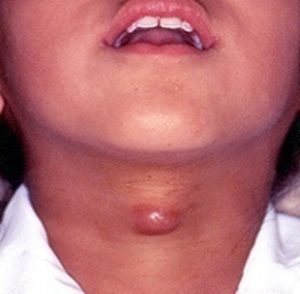 Thyroglossal Duct Cyst[/caption] [caption id="attachment_1783" align="alignnone" width="300"]
Thyroglossal Duct Cyst[/caption] [caption id="attachment_1783" align="alignnone" width="300"] Thyroglossal Duct Cyst[/caption] [caption id="attachment_1776" align="alignnone" width="278"]
Thyroglossal Duct Cyst[/caption] [caption id="attachment_1776" align="alignnone" width="278"]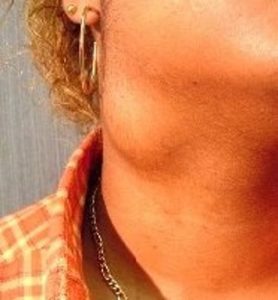 Branchial Cleft Cyst[/caption] [caption id="attachment_1775" align="alignnone" width="263"]
Branchial Cleft Cyst[/caption] [caption id="attachment_1775" align="alignnone" width="263"] Branchial Cleft Cyst[/caption] [caption id="attachment_1774" align="alignnone" width="233"]
Branchial Cleft Cyst[/caption] [caption id="attachment_1774" align="alignnone" width="233"]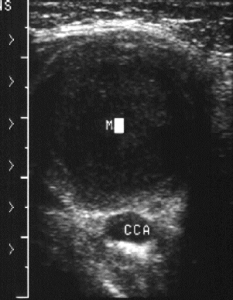 Branchial Cleft Cyst[/caption] [caption id="attachment_1779" align="alignnone" width="300"]
Branchial Cleft Cyst[/caption] [caption id="attachment_1779" align="alignnone" width="300"] Cystic Hygroma[/caption]
Cystic Hygroma[/caption]
[caption id="attachment_1778" align="alignnone" width="235"]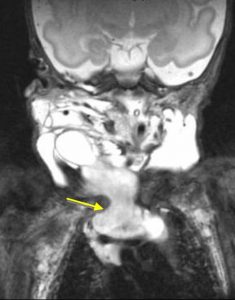 Cystic Hygroma[/caption]
Cystic Hygroma[/caption]
Enepekides DJ. Management of congenital anomalies of the neck. Facial Plast Surg Clin North Am 2001; 9:131.
Lin ST, Tseng FY, Hsu CJ, et al. Thyroglossal duct cyst: a comparison between children and adults. Am J Otolaryngol 2008; 29:83.
Mandell DL. Head and neck anomalies related to the branchial apparatus. Otolaryngol Clin North Am 2000; 33:1309.
Marler JJ, Mulliken JB. Current management of hemangiomas and vascular malformations. Clin Plast Surg 2005; 32:99.
Silverman, J. F., Gurley, A. M., Holbrook, C. T., Joshi, V. V. (1991) Pediatric fine needle aspiration biopsy. American Journal of Clinical Pathology 95: 653–659
Sonnino RE, Spigland N, Laberge JM, Desjardins J, Guttman FM. Unusual patterns of congenital neck masses in children. J Pediatr Surg. 1989 Oct;24(10):966-9.
Selected References
Barnard, et al. Rapid sequence induction of anaesthesia via the intraosseous route: a prospective observational study. Emerg Med J. 2014; Jun 24. pii: emermed-2014-203740.
Jousi M, Saikko S, Nurmi J. Intraosseous blood samples for point-of-care analysis: agreement between intraosseous and arterial analyses. Scand J Trauma Resusc Emerg Med. 2017;25(1):92. Published 2017 Sep 11. doi:10.1186/s13049-017-0435-4
Knuth, et al. Intraosseous Injection of Iodinated Computed Tomography Contrast Agent in an Adult Blunt Trauma Patient. Annals of Emergency Medicine. 2011; 57 (4) 382-386
Miller LJ. et al A new study of intraosseous blood for laboratory analysis.Arch Pathol Lab Med. 2010 Sep;134(9):1253-60.
Miller, et al. Utility of an intraosseous vascular system to deliver contrast dye using a power injector for computerized tomography studies. Annals of Emergency Medicine. 2011; 58 (4) 240-241.
Selected References
Aravindhan N, Chisholm DG. Sulfhemoglobinemia presenting as pulse oximetry desaturations. Anesthesiology. 2000;93:883–884.
So T-Y et al. Topical Benzocaine-induced Methemoglobinemia in the Pediatric Population. J Pediatr Health Care. 22(6):335–339.
Failure to Thrive (FTT) is not just for the clinics. We need to be on the lookout, because if we find it, there is already a big problem.
Definitions of Failure to Thrive may quibble on the details, but for us in the ED:
We can get around the longitudinal requirement by looking at weight as a "spot check" -- if grossly below weight without any other chronic condition, be alarmed.
Failure to thrive results from inadequate calories. This may be due to:
Any concern should trigger a more complete H&P (in audio).
Classic instructional video on the mother-infant dyad (scan through for various types).
After a focused H&P, you may need to admit the child for further workup, or to show that he can/cannot gain weight with routine care.
Remember, if you are the first one to bring this up, there is a real problem. By definition, an outpatient plan has failed. We will not be able to distinguish among the various possibilities of organic and non-organic causes (or mix thereof); our job is to be ready to catch it and act on it. The child's development, future intelligence, and welfare are at risk.
References
Birth to 24 months: Boys Weight-for-length percentiles and Head circumference-for-age percentiles
Birth to 24 months: Boys Length-for-age percentiles and Weight-for-age percentiles
Birth to 24 months: Girls Weight-for-length percentiles and Head circumference-for-age percentiles
Birth to 24 months: Girls Length-for-age percentiles and Weight-for-age percentiles
Jaffe AC. Failure to Thrive. Pediatrics in Review. 2011; 32(3)
Prutsky GJ et al. When Developmental Delay and Failure to Thrive Are Not Psychosocial. Hospital Pediatrics. 2016; (1):6
No one ever wants to find himself in this situation. A factory explodes. A building catches fire. A multi-vehicle traffic collision. Or an act of terrorism.
Very quickly, we have to scrap business as usual. We have to adapt to our new circumstances.
Definition of a mass casualty incident (MCI):
An incident which produces multiple casualties such that emergency services, medical personnel and referral systems within the normal catchment area cannot provide adequate and timely response and care without unacceptable mortality and/or morbidity.
In other words, our demand far outpaces our resources.
"If you can hear the sound of my voice, follow me". Those patients are GREEN, minor.
Otherwise, we need a system to distinguish those who can be DELAYED, IMMEDIATE, or EXPECTANT (soon to be deceased).
Use Simple Triage and Rapid Treatment (START) for 8 or older, JumpSTART for less than 8 years of age.

For Older Children, Adolescents, and Adults (8 or greater) -- START:
For Children less than 8 years of age (Infants Use Pediatric Assessment Triangle) -- JumpSTART:

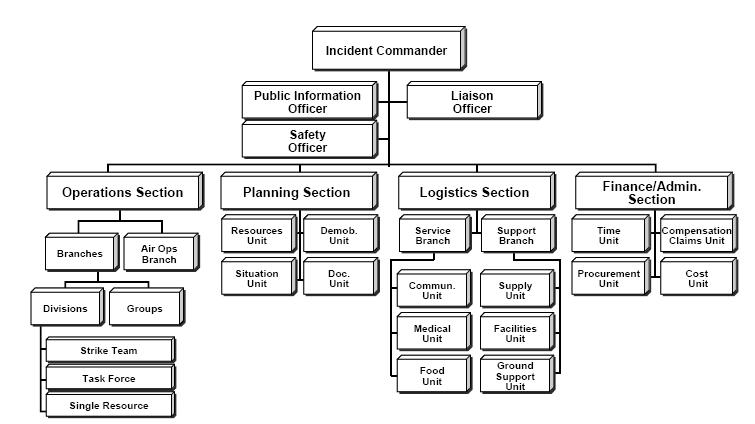 MCI Organizational Chart
MCI Organizational ChartSelected References
Briggs SM. Disaster management teams. Curr Opin Crit Care. 2005 Dec;11(6):585-
Culley JM, Svendsen E. A review of the literature on the validity of mass casualty triage systems with a focus on chemical exposures. American journal of disaster medicine. 2014; 9(2):137-150
FEMA IS 0100.b - Introduction to the Incident Command System (ICS), Student Manual. http://training.fema.gov/emiweb/is/is100b/student%20manual/02ics100b_sm_october2013.pdf. Accessed 03 MAY 2019.
Jensen J, Youngs G. Explaining implementation behaviour of the National Incident Management System (NIMS). Disasters. 2015 Apr;39(2):362-88. doi: 10.1111/disa.12103.
Lee JS, Franc JM. Impact of a Two-step Emergency Department Triage Model with START, then CTAS, on Patient Flow During a Simulated Mass-casualty Incident. Prehosp Disaster Med. 2015 Jun 24:1-7.
Lerner EB, Schwartz RB, Coule PL, et al. "Mass Casualty Triage: An Evaluation of the Data and Development of a Proposed National Guideline." Disaster Medicine and Public Health Preparedness 2(Suppl. 1) 2008, pp S25-S34.