Categories
Most newborns will have some jaundice. Most jaundice is benign.
So, how can we sort through the various presentations and keep our newborns safe?
Pathologic Jaundice
When a baby is born with jaundice, it’s always bad. This is pathologic jaundice, and it’s almost always caught before the baby goes home. Think about ABO-incompatbility, G6PD deficiency, Crigler-Najjar, metabolic disturbances, and infections to name a few. Newborns are typically screened and managed.
Physiologic Jaundice
Physiologic jaundice, on the other hand, is usually fine, until it’s not.
All babies have some inclination to develop jaundice. Their livers are immature. They may get a little dehydrated, especially if mother’s milk is late to come in. In today’s practice, we are challenged to catch those at risk for developing complications from rising bilirubin levels.
Hyperbilirubinemia is the result of at least one of three processes: you make too much, you don’t process it enough, or you don’t get rid of it fast enough.
Increased production
Bilirubin mostly comes from the recycling of red blood cells. Heme is broken down in in the liver and spleen to biliverdin then bilirubin.
Normal, full term babies without jaundice run a little high -- bilirubin production is two to three times higher than in adults, because they are born with a higher hematocrit. Also, fetal hemoglobin is great at holding on to oxygen, but has a shorter life span, and high turn-over rate, producing more bilirubin.
Impaired conjugation
Think of bilirubin as your email. Unconjugated bilirubin is your unread email. To process it or get rid of it – you have to open it. Of course, the more unread messages that accumulate, the more unwell you feel.
Conjugated bilirubin is your opened and processed email. So much easier to sort out, deal with, and get rid of.
Decreased excretion
Both unread email and unconjugated bilirubin continue to float around in your inbox. Unconjugated bilirubin keeps getting reabsorbed in the intestinal mucosa through enterohepatic circulation.
Processed email and conjugated bilirubin are easier to sort out. Conjugated bilirubin is water soluble, so it goes right into the read folder in your gallbladder, and is excreted off your inbox. Later on down the line in the intestine, conjugated bilirubin can’t be reabsorbed through the intestinal mucosa. Like when you open an email and forget about it – it passes on through, out of your system.
Newborns are terrible at answering emails. There is a lot of unread unconjugated bilirubin is floating around. The liver and spleen are just not able to keep up.
Also, newborns have a double-whammy administrative load. Normally, bacteria in the gut can further break down conjugated bilirubin to urobilin and get excreted in the urine. The infant’s gut is relatively sterile, so no admin assistance there. Just to add to the workload a poor little newborn has to do – he is being sabotaged by extra beta-glucuronidase which will take his hard-earned conjugated bilirubin and unconjugate it again, then recycle it, just like email you “mark as unread”.
How Does this All Go Down?
The recommended followup is 48 hours after discharge from the nursery for a routine bilirubin check, often in clinic, and often via the transcutaneous route.
More Specifically:
| Infant Discharged | Should Be Seen by Age |
| Before age 24 h | 72 h |
| Between 24 and 48 h | 96 h |
| Between 48 and 72 h | 120 h |
The neonate will end up in your ED off hours, if there is concern, if his status deteriorates, or simply by chance. We need to know how to manage this presentation, because time is of the essence to avoid complications if hyperbilirubinemia is present.
Critical Action #1:
Assess risk for developing severe hyperbilirubinemia.
This will tell you: check now in ED or defer to clinic (default is to check).
| Risk Factors for Developing Hyperbilirubinemia |
| Total serum bilirubin/Transcutaneous bilirubin in high-risk zone |
| Jaundice in first 24 hours |
| ABO incompatibility with positive direct Coombs, known hemolytic disease, or elevated ETCO |
| Gestational age 35-36 weeks |
| Prior sibling had phototherapy |
| Cephalohematoma or bruising |
| Exclusive breastfeeding, especially with poor feeding or weight loss |
| East Asian Race |
Critical Action #2
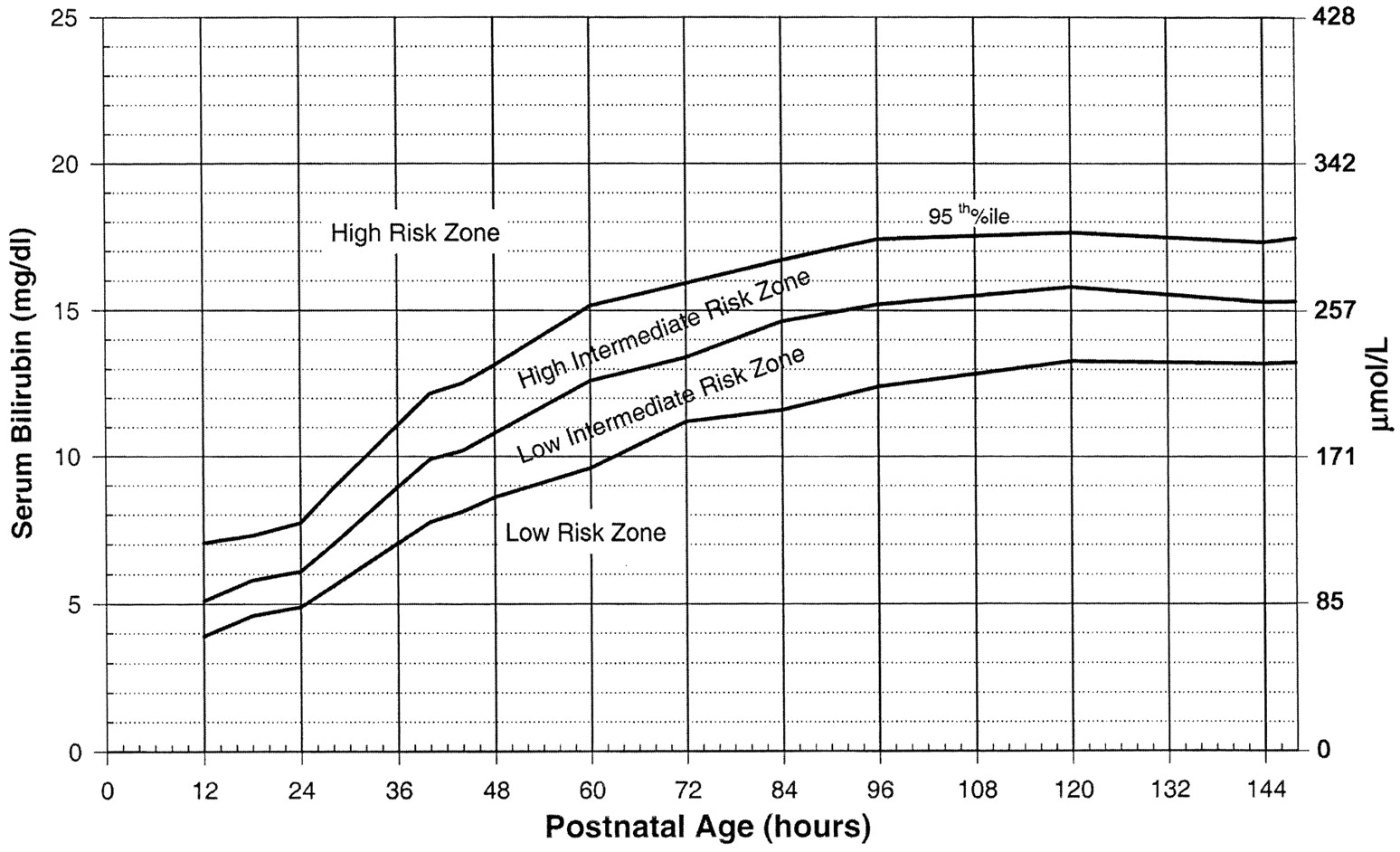
Check bilirubin and match this with how old the child is -- in hours of life -- at the time of bilirubin measurement.
This will tell you: home or admission.
Use the Bilitool or Bhutani Nomogram (below).
Can I go Home Now?
In general, babies at low-risk and low-intermediate risk can go home (see below). Babies at high-intermediate or high risk are admitted (see below).
Critical Action #3:
Assess risk for developing subsequent neurotoxicity.
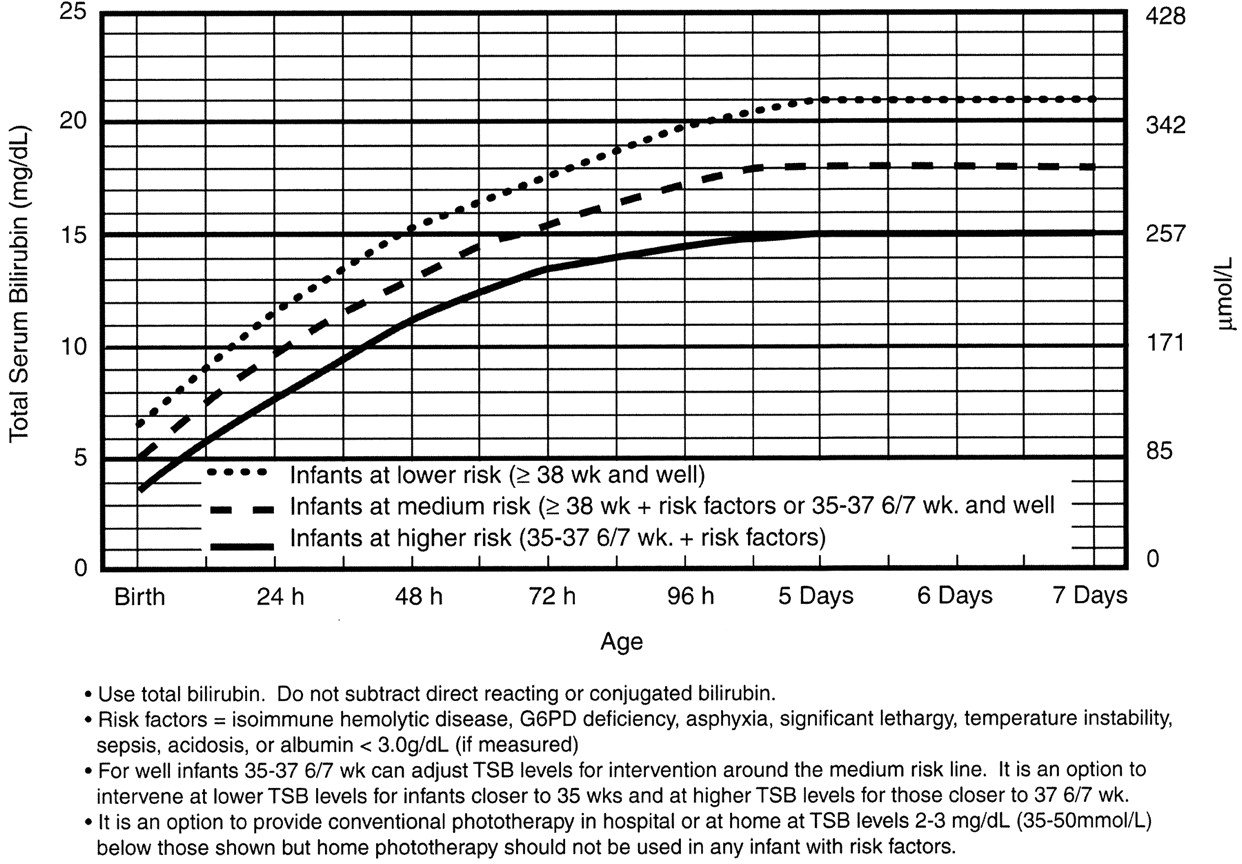
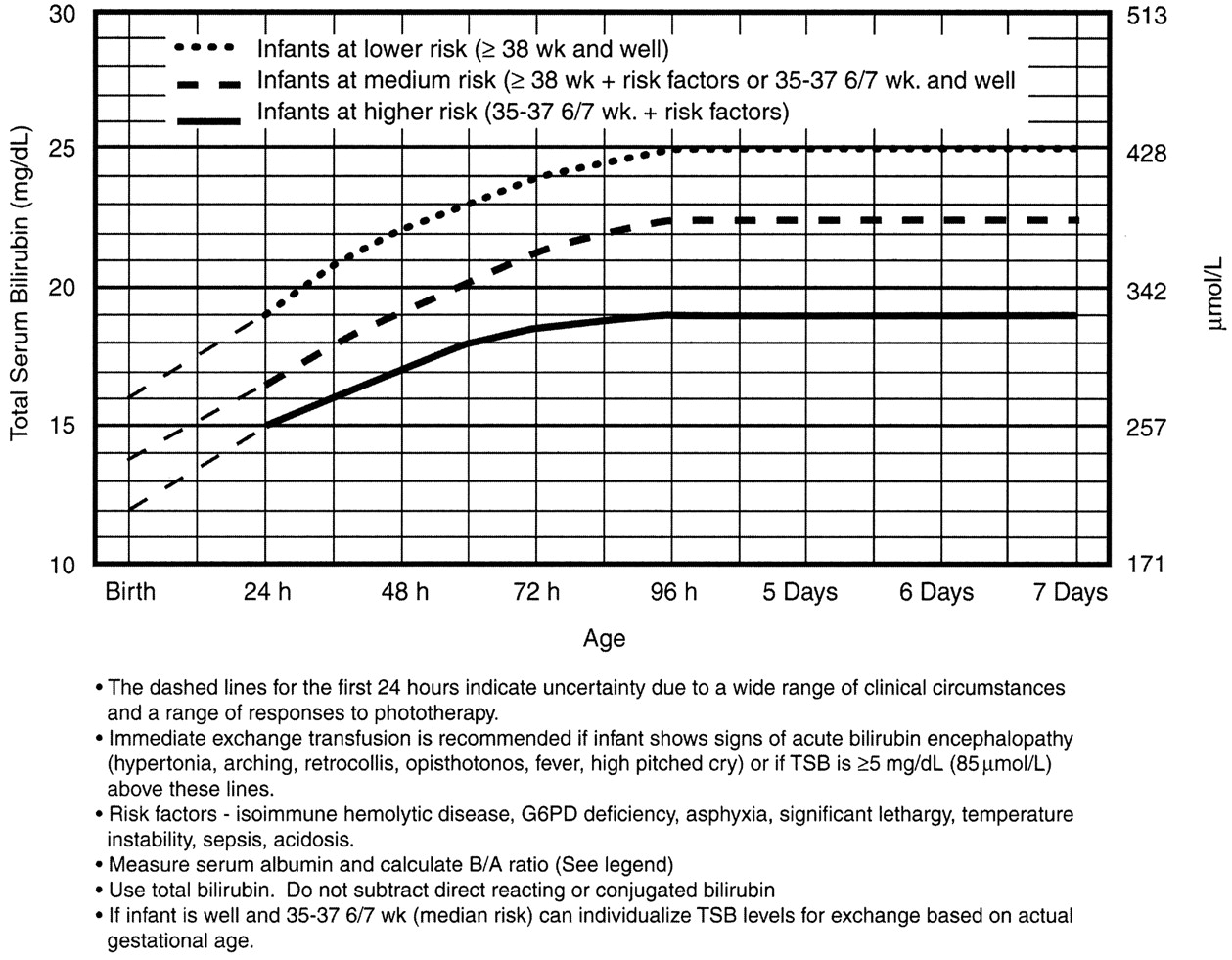
This will tell you: a) phototherapy or b) exchange transfusion
Phototherapy Now?
Exchange Transfusion Now?
Home care
The neonate who is safe to go home is well appearing, and not dehydrated. His total bilirubin is in the low to low-intermediate risk for developing severe hyperbilirubinemia, and he is not at high risk for neurotoxicity based on risk factors.
Babies need to stay hydrated. Breast feeding mothers need encouragement and need to offer feeds 8-12 times/day – an exhausting regimen. The main message is: stick with it. Make sure to enlist the family's help and support to keep Mom hydrated, eating well, and resting whenever she can. Supplementing with formula or expressed breast milk is not routinely needed. Be explicit that the neonate should not receive water or sugar water – it can cause dangerous hyponatremia. A moment of solid precautionary advice could avert a disaster in the making.
The child’s pediatrician will help more with this, and you can remind nursing mothers of the excellent La Leche League – an international group for breastfeeding support. They have local groups everywhere, including a hotline to call.
Nursery Care
If the baby is at high intermediate or high risk for hyperbilirubinemia, then he should be admitted for hydration, often IV. Most babies with hyperbilirubinemia are dehydrated, which just exacerbates the problem.
Bililights or biliblankets, provide the baby with the right blue spectrum of light to isomerize bilirubin to the more soluble form. Traditionally, we have thought them to be more effective or safer than filtered sunlight. A recent randomized control trial by Slusher et al. in the New England Journal of Medicine compared filtered sunlight versus conventional phototherapy for safety and efficacy in a resource-poor environment. These were all term babies with clinically significant jaundice in Nigeria. To standardize the intervention, they used commercial phototherapy canopies that remove most UV rays. None of them became dehydrated or became sunburned. The filtered sunlight resulted in a 93% successful treatment versus 90% for conventional phototherapy. My take away: we now have some evidence basis for using filtered sunlight as an adjunct for babies well enough to go home.
Critical Care
Although rare, the critically ill neonate with hyperbilirubinemia requires immediate intervention.
He will be dehydrated – possibly in shock. He will be irritable.
Or, he may just have a dangerously high bilirubin level – at any minute he could develop bilirubin induced neurologic dysfunction, or BIND, especially when bilirubin concentrations reach or surpass 25 mg/dL (428 micromol/L). The bilirubin is so concentrated that it leeches past the blood brain barrier and causes neuronal apoptosis. BIND is a spectrum from acute bilirubin encephalopathy to kernicterus, all involving some disorder in vision, hearing, and later gait, speech, and cognition.
Acute bilirubin encephalopathy starts subtly. The neonate may be sleepy but hypotonic or have a high-pitched cry; he maybe irritable or inconsolable, jittery or lethergic.
The dehydration and neurologic dysfnction from the hyperbilirubinemia may even cause fever. Check the bilirubin in any neonate you are working up for sepsis.
Acute bilirubin encephalopathy may progress to an abnormal neurologic exam, seizures, apnea, or coma.
Kernicterus is the final, permanent result of bilirubin encephalpathy. The child may have choreoathetoid cerebral palsy with chorea, tremor, ballismus, and dystonia. He may have sensorineural hearting loss, or cognitive dysfunction.
It is for this reason that any child sick enough to be admitted should be considered for exchange transfusion. Most babies need just a little gentle rehydration and bililights, but to be sure, the admitting team will look at a separate nomogram to gage the child’s risk and decide whether to pull the trigger on exchange transfusion. For our purposes, a ballpark estimate is that if the total serum bilirubin is 5 mg/dL above the phototherapy threshold, or if they have any red flag signs or symptoms, then exchange transfusion should be started.
Exchange transfusion involves taking small aliquots of blood from the baby and replacing them with donor blood. It’s often a manual procedure, done with careful monitoring. It can be done with any combination of umbilical arteries or veins with peripheral arteries or veins. In general, arteries are the output, veins are for transfusion. The baby may need a double-volume exchange, which ends up replacing about 85% of circulating blood, a single-voume exchange, replacing about 60% of blood, or any fraction of that with apartial volume exchange. It is a very delicate procedure that requires multiple hours and often multiple staff.
and replacing them with donor blood. It’s often a manual procedure, done with careful monitoring. It can be done with any combination of umbilical arteries or veins with peripheral arteries or veins. In general, arteries are the output, veins are for transfusion. The baby may need a double-volume exchange, which ends up replacing about 85% of circulating blood, a single-voume exchange, replacing about 60% of blood, or any fraction of that with apartial volume exchange. It is a very delicate procedure that requires multiple hours and often multiple staff.
For our pruposes, just be aware that the jaundiced baby in front of you may need escalation of his care.
Summary
Find out the hour of life of the baby at the time of bilirubin measurement. Identify risk factors for developing severe hyperbilirubinemia and/or neurotoxicity
The child with low to low-intermediate risk may be a good outpatient candidate provided he is well, not dehydrated, and follow-up is assured.
The child with high-intermediate to high-risk for developing severe hyperbilirubinemia should be admitted for hydration, bililights, and/or assessment for exchange transfusion.
The unwell child with or without current neurologic findings should have immediate exchange transfusion.
References
Benitz WE. Hospital Stay for Healthy Term Newborn Infants. Pediatrics. 2015; 135(5):948-53.
Lauer BJ, Spector ND. Hyperbilirubinemia in the Newborn. Pediatrics in Review. 2011; 32(8):341-9.
This post and podcast are dedicated to Gita Pensa, MD, for her commitment to #FOAMed and passion for asynchronous learning and education innovation.