Traditional Approach:

Adolescent with mallet finger and Kirschner wire fixation. Nellans et al. Pediatric Hand Injuires. Hand Clin. 2013 November ; 29(4): 569–578

Lee SA et al. Ultrasonography of the finger. Ultrasonography 2016; 35(2): 110-123.
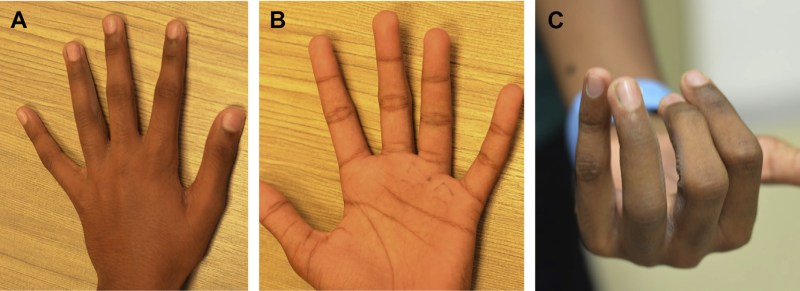
A, B: Relatively normal appearance; C: in flexion, rotational abnormality evident. Liao CY et al. Pediatric Hand and Wrist Fractures. Clin Plastic Surg 46 (2019) 425–436

Mims L et al. Extra-Octave Fracture in a 14-Year-Old Basketball Player. Journal of Pediatrics. 2017; 186: P206-206
Kiely AL et al. The optimal management of Seymour fractures in children and adolescents: a systematic review protocol. Systematic Reviews. 2020; 9 (150).
Liao CY et al. Pediatric Hand and Wrist Fractures. Clin Plastic Surg 46 (2019) 425–436
Lin JS et al. Treatment of Acute Seymour Fractures. J Pediatr Orthop. 2009; 39(1):e23-e27.
Mims L et al. Extra-Octave Fracture in a 14-Year-Old Basketball Player. Journal of Pediatrics. 2017; 186: P206-206
Mohseni M et al. Ulnar Collateral Ligament Injury. Stat Pearls. 2020
Nellans et al. Pediatric Hand Injuires. Hand Clin. 2013 November ; 29(4): 569–578
Pattni A et al. Volar Plate Avulsion Injury. Eplasty. 2016; 16: ic22.
Stevenson J et al. The use of prophylactic flucloxacillin in treatment of open fractures of the distal phalanx within an accident and emergency department: a double-blind randomized placebo-controlled trial. The Journal of Hand Surgery: British & European. 2003; 28(5): 388-394
Yeh PC et al. Pediatric Hand Fractures. Techniques in Orthopaedics. 2009
| Temperature (core) | Presentation | Management | |
| Miliaria Crystallina | Normal | Salt-colored tiny papules, easily burst; not pruritic | Modify environment; light clothing; hydration |
| Miliaria Rubra | Normal | Discrimiate, red papules, not assocaited with follicles; pruritic | Above plus cool compresses; calamine lotion; symptomatic tx for pruritis |
| Miliaria Profunda | Normal | Confluent flesh-colored, “lumpy-bumpy”; burning | Same as rubra |
| Miliaria Pustulosa | Normal | May resemble rubra and/or crustallina, but pustular; h/o previous dermatitis | Same as above, but may may need antibiotic if no improvement over time |
| Heat edema | Normal | Swelling of feet, ankles, and/or lower legs | Modify environment; elevate legs |
| Heat syncope | Normal | Dizziness, orthostatic hypotension, and syncope after exertion with rapid return to normal mental status when supine | Modify environment; rehydration; monitoring |
| Heat cramps | May be elevated to 40°C (104°F) | Exercise-induced cramping in large muscle groups, especially legs | Hydration; consider labs (Cr, total CK); may counsel to stretch muscles passively, gently |
| Heat tetany | May be elevated to 40°C (104°F) | Hyperventilation with paresthesia, carpopedal spasm | Modify environment; hydration; may place non-rebreather mask on low (or off) for rebreathing CO2 |
| Heat exhaustion | Elevated up to 40°C (104°F) | Normal mental status, fatigue, that rapidly improves with treatment; tachycardia; GI symptoms; electrolyte abnormalities | Cool environment; hydration; consider labs with severe symptoms, or if not improved |
| Heat Stroke | >40 to 40.5°C (104 to 105°F) | Altered mental status; tachypneic; tachycardic with hypotension; electrolyte abnormalities; GI symptoms; often with renal failure, rhabdomyloysis, renal failure; possibly with cardiogenic shock or ARDS or DIC | Rapid cooling with all modalities available (radiation, conduction, convection, evaporation); IV rehydration; labs; monitoring; ICU admission |
 Miliaria Crystallina
Miliaria Crystallina  Miliaria Crystallina — Infant
Miliaria Crystallina — Infant  Miliaria Crystallina — Older Child
Miliaria Crystallina — Older Child  Miliaria Rubra — Infant
Miliaria Rubra — Infant  Miliaria Rubra — Infant
Miliaria Rubra — Infant  Miliaria Rubra — Toddler
Miliaria Rubra — Toddler  Miliaria Rubra — Adolescent
Miliaria Rubra — Adolescent  Miliaria Profunda
Miliaria Profunda Selected References
Bergeron MF, Devore C, et al. Council on Sports Medicine and Fitness and Council on School Health, Policy statement—Climatic heat stress and exercising children and adolescents. Pediatrics 2011; 128:e741.
Casa DJ et al. The Inter-Association Task Force for Preventing Sudden Death in Secondary School Athletics Programs: Best-Practices Recommendations. J Athl Train. 2013 Jul-Aug; 48(4): 546–553.
DeFranco MJ et al. Environmental issues for team physicians. Am J Sports Med. 2008 Nov;36(11):2226-37.
Ishimine P. Hyperthermia. In: Pediatric Emergency Medicine, Baren JM, Rothrock SG, Brennan JA, Brown L (Eds), Saunders Elsevier, Philadelphia 2008. p.992.
Jardine DS. Heat illness and heat stroke. Pediatr Rev 2007; 28:249.
Ask yourself -- again -- why is this not... appendicitis-torsion-intussusception-etc.
Admit sick children, but most go home, so...




Selected References
Khan WA et al. Central Nervous System Manifestations of Childhood Shigellosis: Prevalence, Risk Factors, and Outcome. Pediatrics. 1999 Feb;103(2):E18
Lee JY et al. Diagnostic yield of stool culture and predictive factors for positive culture in patients with diarrheal illness. Medicine (Baltimore). 2017 Jul; 96(30): e7641.
Nelson JD et al. Treatment of Salmonella gastroenteritis with ampicillin, amoxicillin, or placebo. Pediatrics 1980; 65:1125.

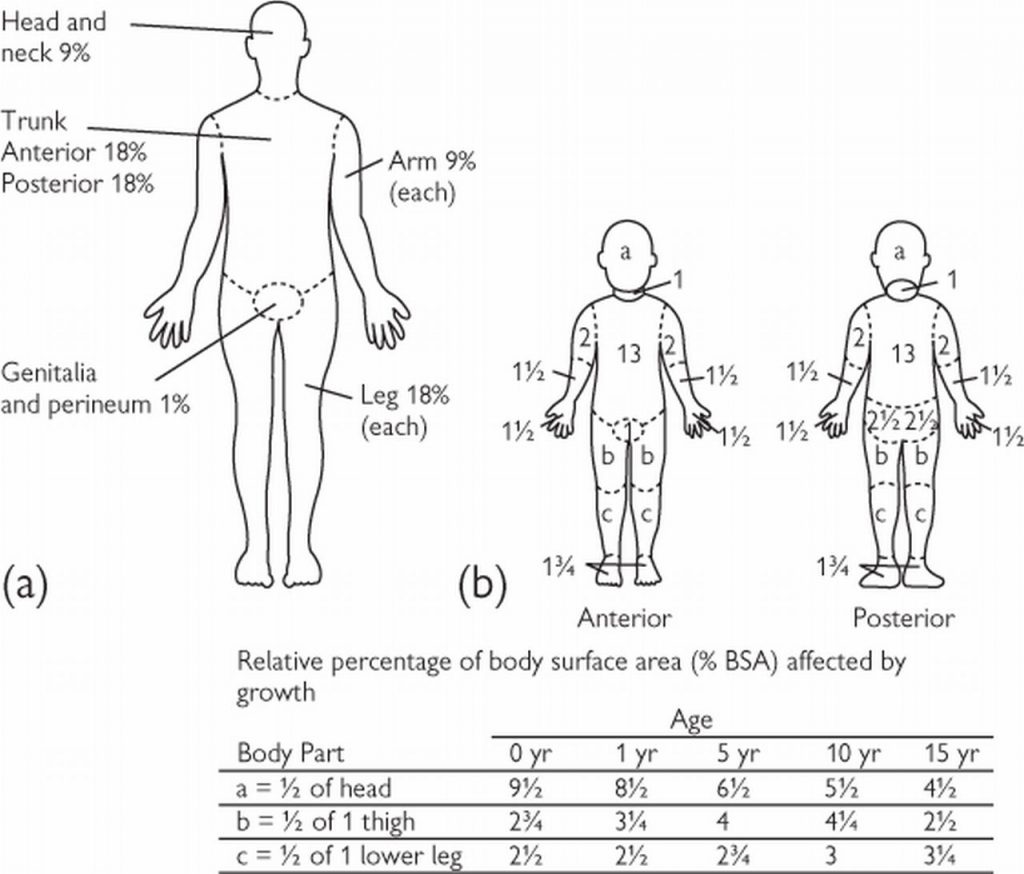
Amount needed in addition to maintenance fluids:
Add 1/2 of X to maintenance over the 1st 8 hours
Add the other 1/2 of X to maintenance over the next 16 hours
Selected References
Mahar PD et al. Clinical differences between major burns patients deemed survivable and non-survivable on admisssion. Injury. 2015; 46:870-873.
Mathis E et al. Pediatric Thermal Burns and Treatment: A Review of Progress and Future Prospects. Medicines. 2017; 4:91.
Osuka A et al. Glycocalyx shedding is anhanced by age and correlates with increased fluid requirement in patients with major burns. Shock. 2017; 50(1):60-65.
Sebastian R et al. Percutaneous pigtail catheter in the treatment of pneumothorax in major burns: The best alternative? Burns. 2015; e24-227
Sherren PB et al. Lethal triad in severe burns. Burns. 2014; 1492-1496.
Strobel AM et al. Emergency Care of Pediatric Burns. Emerg Med Clin N AM. 2018; 441-458.