Traditional Approach:
Hernia
Myth: “If it’s not strangulated, it’s elective”
Reality: Unlike in adults, all hernias in children are repaired at the time of diagnosis because:
Most groin hernias in children are indirect inguinal hernias (incomplete closure of processus vaginalis).
Most indirect hernias are in boys (10-fold risk), and on the right (60%). Premature babies are at higher risk as well. 15% are bilateral.
Hernias often bulge further with crying. For infants, in supine position, gently restrain their feet on the gurney. They hate it and will cry. For older children, have them laugh, cough, or blow through a syringe.
The “silk glove sign” is not reliable, but if found is highly suggestive of an inguinal hernia. Roll the cord structures across the pubic tubercle. If you feel catching, like two sheets of silk rubbed together, this suggests edema from the patent processus vaginalis.
Most (80%) incarcerated hernias can be reduced initially and admitted for surgery 24-48 hours after edema has improved. Use age- and patient-appropriate sedation and reduce if no peritonitis or concern for strangulation.
Hydroceles usually are: non-communicating (with the abdomen); worse with crying or during the day; improve by morning; and self-resolve by age 2 without intervention. Communicating hydroceles are: usually present at birth; are associated with a patent processus vaginalis; and are often repaired later, if not resolved by 1 or 2 years of age.
Girls may have an ovary incarcerated in hernial sac.
Open repair or laparoscopic techniques are used. The laparoscope offers visualization of the contralateral side without significant risk of injury to vas deferens.
A metachronous hernia develops later on the other side. Some surgeons opt to explore both sides at the time of diagnosis, others take conservative approach (small risk of fertility issues if both are open-explored)
My take: regardless of presentation, needs admission
Selected References
Abdulhai S, Glenn IC, Ponsky TA. Inguinal Hernia. Clin Perinatol. 2017 Dec;44(4):865-877
Brandt ML. Pediatric hernias. Surg Clin North Am. 2008 Feb;88(1):27-43, vii-viii. doi: 10.1016/j.suc.2007.11.006.
Esposito C, Escolino M, Cortese G, Aprea G, Turrà F, Farina A, Roberti A, Cerulo M, Settimi A. Twenty-year experience with laparoscopic inguinal hernia repair in infants and children: considerations and results on 1833 hernia repairs. Surg Endosc. 2017 Mar;31(3):1461-1468.
Olesen CS, Mortensen LQ, Öberg S, Rosenberg J. Risk of incarceration in children with inguinal hernia: a systematic review. Hernia. 2019 Apr;23(2):245-254
Chances are, you’d be right to chalk up the pain to functional constipation — 90% of pediatric constipation is functional, multifactorial, and mostly benign — as long as it is addressed.
We’re not here for “chances are“; we’re here for “why isn’t it?“
Ask yourself, could it be:
Anatomic malformations: anal stenosis, anterior displaced anus, sacral hematoma
Metabolic: hypothyroidism, hypercalcemia, hypokalemia, cystic fibrosis, diabetes mellitus, gluten enteropathy
Neuropathic: spinal cord abnormalities, trauma, tethered cord
Neuromuscular: Hirschprung disease, intestinal neuronal dysplasia, myopathies, Down syndrome, prune belly syndrome
Connective tissue disorders: scleroderma, SLE, Ehlers-Danlos syndrome
Drugs: opioids, antacids, antihypertensives, anticholinergics, antidepressants, sympathomimetics
Ingestions: heavy metals, vitamin D overload, botulism, cow’s milk protein intolerance
Failure to thrive
Abdominal distention
Lack of lumbosacral curve
Midline pigmentation abnormalities of the lower spine
Tight, empty rectum in presence of a palpable fecal mass
Gush of fluid or air from rectum on withdrawal of finger
Absent anal wink

You gotta push the boat out of the mud before you pray for rain.
— Coach
Polyethylene Glycol (PEG) 3350 (Miralax): 1 to 1.5 g/kg PO daily for 3 to 6 consecutive days. Maximum daily dose: 100 g/day PO. Follow-up with maintenance dose (below) for at least 2 months (usually 6 months)
Lactulose: 1.33 g/kg/dose (2 mL/kg) PO twice daily for 7 days
Mineral Oil (school-aged children): 3 mL/kg PO twice daily for 7 days
Polyethylene Glycol (PEG) 3350 (Miralax): 0.2 to 0.8 g/kg/day PO. Maximum daily dose: 17 g/day. Maintenance dosing for Miralax may need to be tailored; up to 1 g/day maintenance.
Lactulose: 1 to 2 g/kg/day (1.5 to 3 mL/kg/day)PO divided once or twice daily. Maximum daily dose: 60 mL/day in adults.
Mineral Oil: 1 to 3 mL/kg/day PO divided in 1 to 2 doses; maximum daily dose: 90 mL/day
Docusate (Colace): 5 mg/kg/day PO divided QD, BID, or TID (typical adult dose 100 mg BID)
Senna, Bisocodyl — complicated regimens; use your local reference
Selected References
Freedman SB et al. Pediatric Constipation in the Emergency Department: Evaluation, Treatment, and Outcomes. JPGN 2014;59: 327–333.
North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition. Clinical Practice Guideline: Evaluation and Treatment of Constipation in Infants and Children. JPGN 2006; 43:e1-e13.
Tabbers MM et al. Evaluation and Treatment of Functional Constipation in Infants and Children: Evidence-Based Recommendations From ESPGHAN and NASPGHAN. JPGN 2014;58: 258–274.

Adolescent with mallet finger and Kirschner wire fixation. Nellans et al. Pediatric Hand Injuires. Hand Clin. 2013 November ; 29(4): 569–578

Lee SA et al. Ultrasonography of the finger. Ultrasonography 2016; 35(2): 110-123.
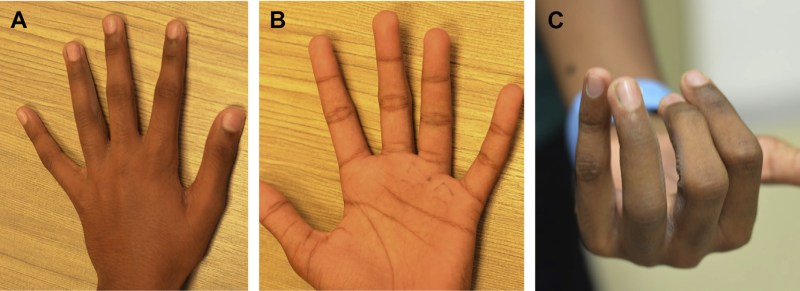
A, B: Relatively normal appearance; C: in flexion, rotational abnormality evident. Liao CY et al. Pediatric Hand and Wrist Fractures. Clin Plastic Surg 46 (2019) 425–436

Mims L et al. Extra-Octave Fracture in a 14-Year-Old Basketball Player. Journal of Pediatrics. 2017; 186: P206-206
Kiely AL et al. The optimal management of Seymour fractures in children and adolescents: a systematic review protocol. Systematic Reviews. 2020; 9 (150).
Liao CY et al. Pediatric Hand and Wrist Fractures. Clin Plastic Surg 46 (2019) 425–436
Lin JS et al. Treatment of Acute Seymour Fractures. J Pediatr Orthop. 2009; 39(1):e23-e27.
Mims L et al. Extra-Octave Fracture in a 14-Year-Old Basketball Player. Journal of Pediatrics. 2017; 186: P206-206
Mohseni M et al. Ulnar Collateral Ligament Injury. Stat Pearls. 2020
Nellans et al. Pediatric Hand Injuires. Hand Clin. 2013 November ; 29(4): 569–578
Pattni A et al. Volar Plate Avulsion Injury. Eplasty. 2016; 16: ic22.
Stevenson J et al. The use of prophylactic flucloxacillin in treatment of open fractures of the distal phalanx within an accident and emergency department: a double-blind randomized placebo-controlled trial. The Journal of Hand Surgery: British & European. 2003; 28(5): 388-394
Yeh PC et al. Pediatric Hand Fractures. Techniques in Orthopaedics. 2009
| Temperature (core) | Presentation | Management | |
| Miliaria Crystallina | Normal | Salt-colored tiny papules, easily burst; not pruritic | Modify environment; light clothing; hydration |
| Miliaria Rubra | Normal | Discrimiate, red papules, not assocaited with follicles; pruritic | Above plus cool compresses; calamine lotion; symptomatic tx for pruritis |
| Miliaria Profunda | Normal | Confluent flesh-colored, “lumpy-bumpy”; burning | Same as rubra |
| Miliaria Pustulosa | Normal | May resemble rubra and/or crustallina, but pustular; h/o previous dermatitis | Same as above, but may may need antibiotic if no improvement over time |
| Heat edema | Normal | Swelling of feet, ankles, and/or lower legs | Modify environment; elevate legs |
| Heat syncope | Normal | Dizziness, orthostatic hypotension, and syncope after exertion with rapid return to normal mental status when supine | Modify environment; rehydration; monitoring |
| Heat cramps | May be elevated to 40°C (104°F) | Exercise-induced cramping in large muscle groups, especially legs | Hydration; consider labs (Cr, total CK); may counsel to stretch muscles passively, gently |
| Heat tetany | May be elevated to 40°C (104°F) | Hyperventilation with paresthesia, carpopedal spasm | Modify environment; hydration; may place non-rebreather mask on low (or off) for rebreathing CO2 |
| Heat exhaustion | Elevated up to 40°C (104°F) | Normal mental status, fatigue, that rapidly improves with treatment; tachycardia; GI symptoms; electrolyte abnormalities | Cool environment; hydration; consider labs with severe symptoms, or if not improved |
| Heat Stroke | >40 to 40.5°C (104 to 105°F) | Altered mental status; tachypneic; tachycardic with hypotension; electrolyte abnormalities; GI symptoms; often with renal failure, rhabdomyloysis, renal failure; possibly with cardiogenic shock or ARDS or DIC | Rapid cooling with all modalities available (radiation, conduction, convection, evaporation); IV rehydration; labs; monitoring; ICU admission |
 Miliaria Crystallina
Miliaria Crystallina  Miliaria Crystallina — Infant
Miliaria Crystallina — Infant  Miliaria Crystallina — Older Child
Miliaria Crystallina — Older Child  Miliaria Rubra — Infant
Miliaria Rubra — Infant  Miliaria Rubra — Infant
Miliaria Rubra — Infant  Miliaria Rubra — Toddler
Miliaria Rubra — Toddler  Miliaria Rubra — Adolescent
Miliaria Rubra — Adolescent  Miliaria Profunda
Miliaria Profunda Selected References
Bergeron MF, Devore C, et al. Council on Sports Medicine and Fitness and Council on School Health, Policy statement—Climatic heat stress and exercising children and adolescents. Pediatrics 2011; 128:e741.
Casa DJ et al. The Inter-Association Task Force for Preventing Sudden Death in Secondary School Athletics Programs: Best-Practices Recommendations. J Athl Train. 2013 Jul-Aug; 48(4): 546–553.
DeFranco MJ et al. Environmental issues for team physicians. Am J Sports Med. 2008 Nov;36(11):2226-37.
Ishimine P. Hyperthermia. In: Pediatric Emergency Medicine, Baren JM, Rothrock SG, Brennan JA, Brown L (Eds), Saunders Elsevier, Philadelphia 2008. p.992.
Jardine DS. Heat illness and heat stroke. Pediatr Rev 2007; 28:249.
Ask yourself -- again -- why is this not... appendicitis-torsion-intussusception-etc.
Admit sick children, but most go home, so...




Selected References
Khan WA et al. Central Nervous System Manifestations of Childhood Shigellosis: Prevalence, Risk Factors, and Outcome. Pediatrics. 1999 Feb;103(2):E18
Lee JY et al. Diagnostic yield of stool culture and predictive factors for positive culture in patients with diarrheal illness. Medicine (Baltimore). 2017 Jul; 96(30): e7641.
Nelson JD et al. Treatment of Salmonella gastroenteritis with ampicillin, amoxicillin, or placebo. Pediatrics 1980; 65:1125.

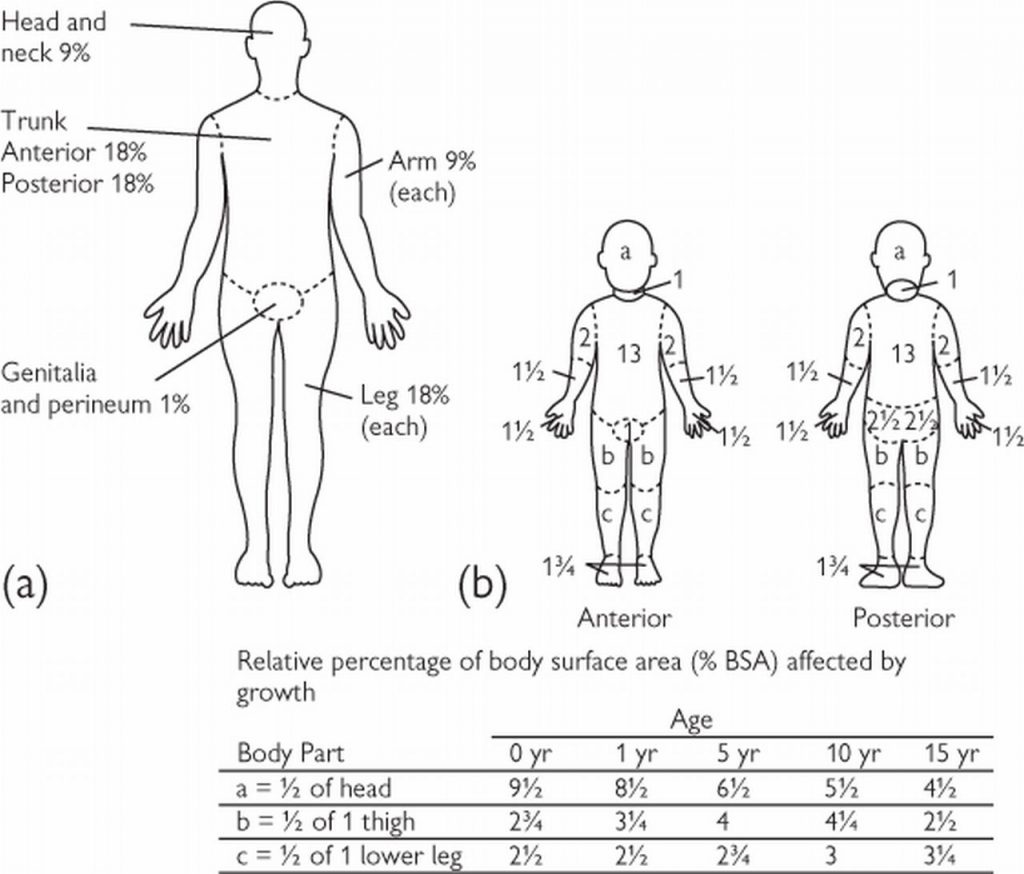
Amount needed in addition to maintenance fluids:
Add 1/2 of X to maintenance over the 1st 8 hours
Add the other 1/2 of X to maintenance over the next 16 hours
Selected References
Mahar PD et al. Clinical differences between major burns patients deemed survivable and non-survivable on admisssion. Injury. 2015; 46:870-873.
Mathis E et al. Pediatric Thermal Burns and Treatment: A Review of Progress and Future Prospects. Medicines. 2017; 4:91.
Osuka A et al. Glycocalyx shedding is anhanced by age and correlates with increased fluid requirement in patients with major burns. Shock. 2017; 50(1):60-65.
Sebastian R et al. Percutaneous pigtail catheter in the treatment of pneumothorax in major burns: The best alternative? Burns. 2015; e24-227
Sherren PB et al. Lethal triad in severe burns. Burns. 2014; 1492-1496.
Strobel AM et al. Emergency Care of Pediatric Burns. Emerg Med Clin N AM. 2018; 441-458.

[caption id="attachment_1777" align="alignnone" width="262"]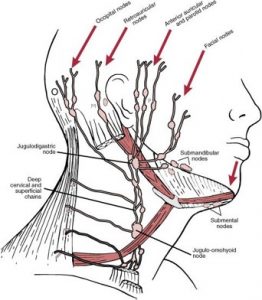 Cervical Node Chain; Lymphadenopathy[/caption] [caption id="attachment_1773" align="alignnone" width="298"]
Cervical Node Chain; Lymphadenopathy[/caption] [caption id="attachment_1773" align="alignnone" width="298"] Bacterial Lymphadenitis[/caption] [caption id="attachment_1772" align="alignnone" width="300"]
Bacterial Lymphadenitis[/caption] [caption id="attachment_1772" align="alignnone" width="300"]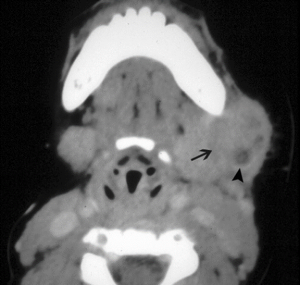 Bacterial lymphadenitis with small abscess[/caption] [caption id="attachment_1771" align="alignnone" width="300"]
Bacterial lymphadenitis with small abscess[/caption] [caption id="attachment_1771" align="alignnone" width="300"] Large Abscess[/caption]
Large Abscess[/caption]


[caption id="attachment_1784" align="alignnone" width="300"]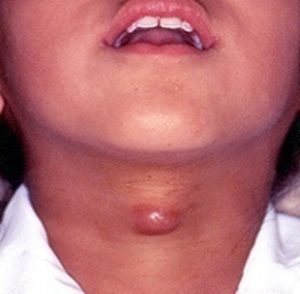 Thyroglossal Duct Cyst[/caption] [caption id="attachment_1783" align="alignnone" width="300"]
Thyroglossal Duct Cyst[/caption] [caption id="attachment_1783" align="alignnone" width="300"] Thyroglossal Duct Cyst[/caption] [caption id="attachment_1776" align="alignnone" width="278"]
Thyroglossal Duct Cyst[/caption] [caption id="attachment_1776" align="alignnone" width="278"]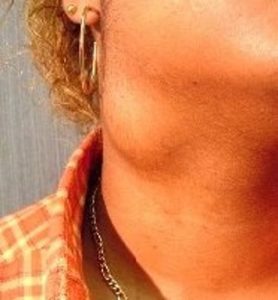 Branchial Cleft Cyst[/caption] [caption id="attachment_1775" align="alignnone" width="263"]
Branchial Cleft Cyst[/caption] [caption id="attachment_1775" align="alignnone" width="263"] Branchial Cleft Cyst[/caption] [caption id="attachment_1774" align="alignnone" width="233"]
Branchial Cleft Cyst[/caption] [caption id="attachment_1774" align="alignnone" width="233"]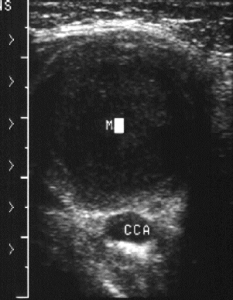 Branchial Cleft Cyst[/caption] [caption id="attachment_1779" align="alignnone" width="300"]
Branchial Cleft Cyst[/caption] [caption id="attachment_1779" align="alignnone" width="300"] Cystic Hygroma[/caption]
Cystic Hygroma[/caption]
[caption id="attachment_1778" align="alignnone" width="235"]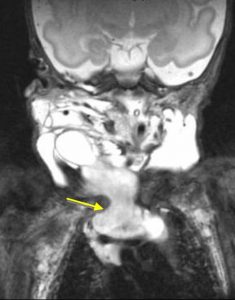 Cystic Hygroma[/caption]
Cystic Hygroma[/caption]
Enepekides DJ. Management of congenital anomalies of the neck. Facial Plast Surg Clin North Am 2001; 9:131.
Lin ST, Tseng FY, Hsu CJ, et al. Thyroglossal duct cyst: a comparison between children and adults. Am J Otolaryngol 2008; 29:83.
Mandell DL. Head and neck anomalies related to the branchial apparatus. Otolaryngol Clin North Am 2000; 33:1309.
Marler JJ, Mulliken JB. Current management of hemangiomas and vascular malformations. Clin Plast Surg 2005; 32:99.
Silverman, J. F., Gurley, A. M., Holbrook, C. T., Joshi, V. V. (1991) Pediatric fine needle aspiration biopsy. American Journal of Clinical Pathology 95: 653–659
Sonnino RE, Spigland N, Laberge JM, Desjardins J, Guttman FM. Unusual patterns of congenital neck masses in children. J Pediatr Surg. 1989 Oct;24(10):966-9.